Updated Guide to CBD and Depression Research

It couldn't have come at a better time.
As we're writing these words, shelter-in-place is very much the daily theme.
A study yesterday said that anti-anxiety med prescriptions were up 34%.
Many people are going to experience an abusive relationship with benzos that we did (see CBD versus benzos for anxiety).
On the depression side, the go-to is SSRIs which boost serotonin.
That's a whole other dance which we've covered in detail at our CBD versus SSRIs or how exactly do SSRIs work.
The answer to the last question is very fascinating for our look at depression and CBD (along with other substances that have popped out in research which we'll look at below).
If SSRIs work for roughly 30% of people, build tolerance, and have a host of other side effects, are their other options?
What does research show for CBD and depression?
Let's dive deep into and along the way, we'll look at new research on depression which is reshaping how it works and how to work against it.
We'll cover these topics:
- New insights on what causes depression
- Brain areas and depression
- Neurotransmitters and depression
- Inflammation and depression
- Neurogenesis and depression
- The new kid on the block...Glutamate and depression
- Hormones and depression (perimenopause)
- Can CBD help with depression?
- Other tools for depression
- How much CBD to take for depression
- What's the best CBD for depression
Okay...lots to cover. Stay with us...there's a payoff.
New insights on what causes depression
We can actually glean a great deal of insight for newer options such as psilocybin, CBD, and NAC (all covered below) and how they work.
They paint depression as a brain in retrenchment...pulling away from itself neuron by neuron.
This can be the result of may different insults:
- Chronic stress
- Inflammation (hyperactive immune)
- Neurotransmitter imbalances (glutamate is a big player as is serotonin - more below)
- Early exposure to infection or chemicals during key periods of brain development
- Drugs and medications
- Trauma

First, understand that the brain is a very dynamic system...changing all the time.
Just by reading this sentence, you're creating a new pathway (albeit brief if never thought of again).
There are very complicated systems in charge of generating new growth (BDNF, serotonin, estrogen/tesosterone, etc) and pruning back old (or not used) growth.
A constant cycle neuron life and death.
As we dived deep into our CBD and addiction (just a sped-up type of learning), there's a balance between these forces of growth and removal.
Interestingly, the endocannabinoid system (where CBD works) is intimately tied into this whole maintenance process along with the immune system of all things.
Endocannabinoids have emerged as mediators of short- and long-term synaptic plasticity in diverse brain structures.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1906867/
Synaptic plasticity refers to this dynamic process of change within the architecture of the brain.
In fact, when they blocked CB1 (our main endocannabinoid receptor) on mice, look at the results:
Mutant mice lacking CB1 receptors show anxiogenic and depressive-like behaviors as well as an altered hypothalamus-pituitary-adrenal axis activity, whereas enhancement of endocannabinoid signaling produces anxiolytic and antidepressant-like effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808114/
Read that back over...when they block endocannabinoid activity, anxiety and depression symptoms occur.
Along with an imbalanced stress response system (HPA).
Enhance the system and anti-anxiety and anti-depressant effects occur.
Curious.
We'll understand why below with the downstream effects of this endocannabinoid system.
Anxiety is an interesting partner in crime since it can result from exact same insults we mentioned above.
Check out CBD and mechanisms of anxiety.
In fact, chronic stress and anxiety can become an insult as well! We'll look at that in the inflammation section.
The take-away is this:
Depression is looking like the net effect of a failure in brain communication and robustness.
We would expect to see signs of this retrenchment in the brain itself from depression.
Let's go there now.
Brain areas and depression
There are three key areas that are really popping up in depression research:
- Hippocampus - seat of memory and mood management
- Thalamus - a relay station between our old and new brain
- Amygdala - seat of emotional processing
Those are the old "reptilian" brain areas.
These are very old (evolutionarily speaking) areas of our brain. Think of them as primitive emotional responses to stimulus.
The new kid on the block is also showing up in depression..the prefrontal cortex.
This is the area right behind your forehead which really makes us human.
One of its tasks is to regulate our emotional brain (the older areas above) and make sense of the signals.
It's the rational head in the room (the room being your brain).
In a well-functioning brain, there's lots of cross-talk between these areas and a balance.
You need to jump when a bus is about to hit you (fight or flight) but not when someone says hello.
It's a tug of war going all the time between these two for a happy balance.
Until it isn't.
If there's reduced activity in one area (such as the prefrontal cortex) or increased in another (amygdala) or even the communication hubs between them, issues arise (anxiety and depression being two possible outcomes).
Research is bearing this out.
First, reduced activity in the prefrontal cortex:
A decreased metabolism in the prefrontal cortex, especially dorsolateral and dorsoventral brain regions, is a frequently replicated finding in MDD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3619732/
MDD is short for major depressive disorder.
Over to the other side, the hippocampus is really coming into focus:
Decreased hippocampal volumes (10, 25) have been noted in subjects with depression.
- Not only does the hippocampus govern memory but it acts as a powerful node or hub for mood.
- Interestingly, the hippocampus may be the most dynamic area of our brain and as a result, the most vulnerable to all the insults we listed above.
After all, every new memory means a change in its structure. It's literally designed to change!
Chronic stress and inflammation is a nightmare for this setup:
The hippocampus, which provides negative feedback regulation of the stress response, is particularly vulnerable to degenerative changes caused by chronic stress.
https://europepmc.org/article/PMC/6758130
In fact, with scans, they can zoom and see the little root-like structures (called dendrites) of the hippocampal neurons shrink:
Repeated psychosocial or restraint stress causes atrophy of apical dendrites in CA3 pyramidal neurons of the hippocampus, accompanied by specific cognitive deficits in spatial learning and memory.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC28422/
The keyword there is "atrophy". To wither.
Folks, this is retrenchment.
The official definition:
reduction in the extent or quantity of something.
To drill down deeper, we find ourselves looking at the neurotransmitters that partially govern this process of brain growth and atrophy.
You'll see how they manage (or mismanage) this process more clearly.
Neurotransmitters and depression
There's been so much focus on this area because Pharma can actually create products from it.
It's not that simple though.
These are very complicated and interwoven pathways.
Like a spiderweb. You push on one area (boost serotonin) and the whole web moves.
In unexpected ways (see Serotonin and suicidal or homicidal thoughts).
That being said, if we can understand how these neurotransmitters really work in terms of supporting our dynamic brain's ongoing remodeling process, it will help you understand what's going on.
Let's start with the main target for the biggest class of antidepressants...serotonin.
SSRIs and SNRIs both target this pathway (with the latter adding on norephedrine).
Most people think of serotonin as the feel-good neurotransmitter but that's belittling at best.
Serotonin is a master regulator in the brain tied to EVERY human behavior you can think of.
Thinking you can just boost serotonin and depression will be gone without any unintended consequences is naive.
Here's the fascinating piece.
SSRIs generally take a few weeks to start to work. Why the delay if boosting serotonin is key for depression?
It turns out that the real effect of boosting serotonin is to increase neurogenesis.
That's a fancy word for building a new brain (and connections)!
Check out CBD and neurogenesis.
In fact, when researchers block the neurogenesis effect from SSRI, look at the result:
In 5HT1A receptors knockout animals treated chronically with fluoxetine, both hippocampal neurogenesis and anxiolytic-like responses were abolished
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648779/
To translate...serotonin (5HT) receptors were blocked for mice who were then given an SSRI (fluoxetine).
The typical neurogenesis and more importantly, the anti-anxiety effects went away!
But wait...there's more (we're not selling steak knives, we promise)...It's even more interesting.
When researchers blocked the CB1 receptor (our endocannabinoid receptor) activity, looked at what happened:
Furthermore, treatment with the SSRI fluoxetine failed to facilitate serotonergic neurotransmission in the prefrontal cortex of CB1 knockout mice activity.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648779/
To translate, when they blocked CB1 activity, fluoxetine (an SSRI - Prozac) lost its serotonin function!
Here's the daisy-chain of events:
- SSRI's boost serotonin
- Serotonin boosts neurogenesis
- Neurogenesis has antidepressant effects
This is all partially mediated via the CB1 receptors.
Check out how SSRIs really work to get the full picture.
So...in the end, SSRI (temporarily since they build tolerance) have their effect via addressing the back-end of our equation...repair and rebuild.
Serotonin can also help on the front end as it governs stress response (see tryptophan and serotonin).
In the end, Serotonin directly boosts BDNF, our brain's fertilizer (see CBD and BDNF) and we'll look at that below in the neurogenesis section.
SSRIs only work for about 30% of people (see CBD versus SSRIs).
Are other neurotransmitters at play? Of course, they are since it's all interconnected.
Dopamine is our reward chemical. Too little function there will definitely affect motivation (is motivation).
Glutamate and GABA are starting to emerge as key players and we'll at separately in its own section (it's that important).
Let's look at some of the insults.
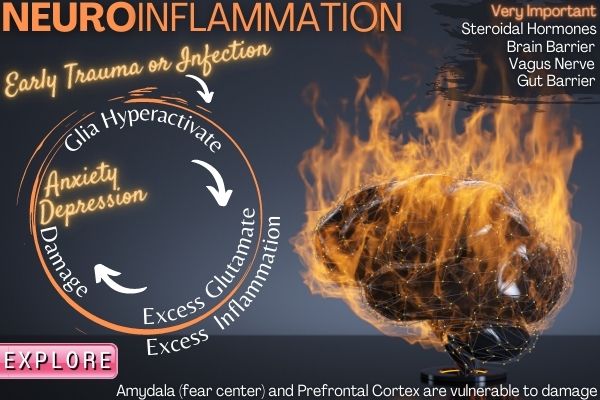
Inflammation, stress, trauma, and depression
Let's look at the insults.
There's lots of research on inflammation and depression.
Such as:
For example, 45% of patients enrolled in a study on treatment-resistant depression had a CRP > 3 mg/L, which is considered high inflammation.
https://www.psychiatrictimes.com/special-reports/five-things-know-about-inflammation-and-depression
Fatigue can also factor in there:
Studies have extensively probed these interactions and found that subjects with depression and fatigue have higher levels of inflammatory immune activation, along with a host of other immunological changes
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6658985/
Inflammation is our immune response. Too much response or chronic hyperactivation to toxic to the brain!
It's a flavor of autoimmune but could also be from early exposure to infection (even in the womb).
A Danish study looked at people who had a serious infection and later developed mood disorders:
People who had been treated for a severe infection were 62% more likely to have developed a mood disorder than those who never had one.
https://www.health.harvard.edu/blog/infection-autoimmune-disease-linked-to-depression-201306176397
People...this is IT for depression.
Early trauma, infection, and stress completely rocks the apple cart later in life.
The link for autoimmune was also high with a 45% increase in the risk of depression.
As for trauma...especially during development:
Childhood trauma is a potent risk factor for developing depression in adulthood, particularly in response to additional stress.
https://pubmed.ncbi.nlm.nih.gov/18602762/
The immune system is turning out to be a major player in a range of mental health issues including depression.
We looked at it in depth at our CBD and neuroinflammation for anxiety review.
From a 30,000 ft view, we have trauma, infection, inflammation, and stress.
If you drill down further, that translates into hyperactivation of immune response, glutamate, stress hormones.
The net effect is an assault on the brain areas we described above...especially the hippocampus and prefrontal cortex.
Key nodes in the depression circuit.
Check out CBD and inflammation for more info.
That's the negative side...let's look at how the brain tries to offset these insults and why THAT side might figure into both depression and helping it.
Neurogenesis and depression
There are many different avenues by which a person may be at risk for depression.
- Maybe their stress response system (serotonin, GABA, etc) isn't as strong.
- Maybe they are subject to chemicals or infection at critical periods of development which leave a mark.
- Maybe their immune system over-responds
- Maybe they have genetic differences that affect certain neurotransmitter levels
Finally...maybe their process for brain repair and growth (neurogenesis) function is below what's needed to keep up with the above!
This is where we can look at things that work and really pinpoint depression's potential resolution.
Let's look at the following in the context of neurogenesis:
- Psilocybin
- NAC
- Mindful meditation
- Exercise
All have shown interesting results in research for depression.
What do they all have in common? They support the neurogenesis pathway.
Psilocybin (the active chemical in magic mushrooms) is a powerful explosion of BDNF (our brain's fertilizer see Psilocybin review).
As this review states:
Atrophy of neurons in the prefrontal cortex (PFC) plays a key role in the pathophysiology of depression and related disorders.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082376/
And magic mushroom's effect?
Serotonergic psychedelics are capable of robustly increasing neuritogenesis and/or spinogenesis both in vitro and in vivo.
Check out the review...there are before/after images of the neuron spines that are amazing to see.
NAC supports the major detox pathway called glutathione (see CBD and glutathione) which is important for handling inflammation, stress, and trauma but it also affects neurogenesis:
Postnatal N-acetylcysteine administration rescues impaired social behaviors and neurogenesis in Slc13a4 haploinsufficient mice.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6557756/
We did a full review of NAC since it was fascinating especially in terms of the glutamate question (more below).
Mindful meditation literally changes the brain structure in key areas tied to depression:
The results suggest that participation in MBSR is associated with changes in gray matter concentration in brain regions involved in learning and memory processes, emotion regulation, self-referential processing, and perspective-taking.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3004979/
Gray matter is the key tracts of communication lines between brain areas. Critical with depression.
And that critical hippocampus area?
In addition, meditators showed significantly larger volumes of the right hippocampus.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184843/
Why does this matter for depression?
Thus, larger volumes in these regions might account for meditators’ singular abilities and habits to cultivate positive emotions, retain emotional stability, and engage in mindful behavior.
Okay...positive emotions...the opposite of depression.
Check out CBD, mindful meditation, and exercise for neurogenesis.
Speaking of exercise...rememember...our body and mind are the same so of course, we have benefits there but why if exercise actually causes inflammation (temporarily)?
As we get older, we lose neurogenesis function. Look at the effects of exercise:
The decline in neurogenesis in aged mice was reversed to 50% of young control levels by running.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1360197/
We drill down deeper and see our old friend, BDNF:
Further research has extended this to show that treadmill exercise in mice and aerobic exercise in humans increases BDNF expression by regulating BDNF gene expression in the hippocampus.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808288/
And there's the hippocampus again.
We covered all of this at CBD and hippocampus neurogenesis.
We'll look specifically at CBD and neurogenesis for depression below.
The net-net is this...we can directly affect this side of the equation for depression. In fact, the more interesting options (psilocybin, NAC, CBD, mindful meditation, etc) all exert their influence here.
Finally, we would expect to see genes tied to some of these pathways to seal the deal.
What does research show there?
Genes tied to depression
Remember the gene above for mice which NAC would help with addressing neurogenesis?
What does it do?
It's a key player in the serotonin pathway called SLC6A4 and it's been tied to major depression.
Tryptophan conversion genes (tryptophan being the precursor to serotonin) have an association as well (see tryptophan and serotonin).
There's a range of serotonin-related genes equally in play. Remember that Serotonin directly boosts BDNF.
Speaking of which, there was also some association with the gene that governs BDNF and depression.
MAO and COMT both degrade or remove neurotransmitters and they are also in play.
Then, there's glutamate...where really exciting new research is focusing.
Depressed females have over-active glutamate receptor gene
https://www.sciencedaily.com/releases/2015/07/150730172348.htm
Let's go there now since there are ways to influence the glutamate pathway. This may be the most important part of this whole review.
The new kid on the block...Glutamate and depression
A quick introduction is in order.
Glutamate is the most active and abundant neurotransmitter in the brain. It's the engine behind EVERYTHING.
Simply put, it's the gas pedal of brain activity. It's the counterpart, GABA, is the brake pedal.
There's a finely tuned and incredibly complex balance between the two with occasional spikes needed (GABA for sleep or glutamate for a test).
Benzos and alcohol pump up GABA levels (see CBD versus Benzos or CBD and alcohol) until they don't. Caffeine, nicotine, and stimulants boost glutamate.
That gives you a good indication of how they work in the brain.
What does any of this have to do with depression?
It's all over it!
- First, too little activity in the prefrontal cortex can feel like depression. Too much glutamate can actually be toxic to neurons!
- Just look at a brain scan of people after a short period of meth usage (the ADHD drugs are amphetamines by the way) to see the holes in brain areas.
Just think about glutamate running wild for a bit...it will start to all make sense.
Let's go back to our various insults from above.
Chronic stress and glutamate
Data from early studies suggest that chronic stress causes prolonged periods of stimulated glutamate release following acute stress exposure, at least in the hippocampus
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3645314/
New research is also showing the prefrontal cortex suffers from excess glutamate which reduces activity.
What about infection, auto-immune, and hyperactive immune response?
Let's introduce microglia, our brain's immune responder. They can be prime to be overactive and the downstream result:
Microglia have the capacity to release a large number of substances that can be detrimental to the surrounding neurons, including glutamate, ATP, and reactive oxygen species.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3630369/
Hyperactivation of microglia (immune response) is tied to a range of mental health illnesses including depression.
That's also the link with early childhood trauma or even in-utero infection.
Of course, there are chemicals and drugs as well.
What originally fascinated us about this pathway was THC's effect on glutamate and NAC's effect on THC addiction.
Our theory is that people who smoke pot chronically are self-medicating to turn down glutamate.
It turns out that THC directly boosts CB1 activity (substitute for anandamide).
CB1's effect on glutamate?
These findings further support the interpretation that CB1 activation leads to a decrease of glutamate release from afferent terminals in the striatum.
https://www.ncbi.nlm.nih.gov/pubmed/11152748
Other brain areas are affected but the striatum is key for addiction, schizophrenia, and other issues.
NAC supports balance in the glutamate system (also very interesting research on addiction and schizophrenia as well as depression).
See NAC review or CBD for addiction or CBD for schizophrenia.
So...the glutamate/GABA balance is a workhorse in brain function and depression.
We'll look at how CBD affects that pathway below.
Next up...depression hit women much harder than men. Why?
Hormones and depression (perimenopause)
We covered this in detail at our CBD and perimenopause depression here but a quick review.
Let's break down how estrogen and progesterone might come into play.
- First, progesterone starts to drop in your early 30's and is at 50% by age 40.
- Estrogen just drops off a cliff around 45-47 during perimenopause
Check out perimenopause versus menopause or why some women get hit so hard by perimenopause.
That transition is what led us to this whole IndigoNaturals research endeavor (that story is here).
So progesterone is a major supporter of GABA function through one of its metabolites, pregnenolone.
If you want a direct tie-in with depression, how about this.
The blockbuster new drug for post-pardum depression is a synthetic version of pregnenolone!
It's been deemed a total game-changer.
You can buy preg in the store here and our full pregnenolone guide. Both men and women have the same levels (don't let the name scare you)
Remember that GABA is the opposing force or constraint on glutamate and we went through its place in the depression landscape above.
Then there's estrogen. Estrogen is our pro-growth hormone and it a huge booster for serotonin function!
One note...in males, testosterone is converted to estrogen in the brain by aromatase.
So glutamate and serotonin. Might be relevant to depression.
This also explains mood changes during the monthly cycle (see CBD for the monthly period).
So when your doctor tells you your hormones are fine for your age, just remember what you're losing with them.
Finally...CBD. Where does it fit into this whole picture?
Can CBD help with depression?
First, CBD is a cannabinoid found in the cannabis plant. It does not produce the "high" like its cousin, THC.
Both interact with a system in our body called the endocannabinoid system which is tasked with governing other key systems:
- Endocrine system - hormones that affect stress response, sleep, and just about everything
- Immune system - inflammatory pathways
- Nervous system - neurotransmitters like serotonin, glutamate, and GABA!
Goodness...we're right in the wheelhouse of depression.
The important aspect appears to be that CBD doesn't just boost or drop levels in any of these pathways in one direction (like SSRIs).
This speaks to why CBD doesn't cause tolerance or addiction (see CBD and tolerance or CBD and addiction).
Let's drill down into the pathways before looking at studies.
- CBD and serotonin for depression
- CBD and glutamate/GABA for depression
- CBD and neurogenesis for depression
- CBD and stress and inflammation response for depression
Let's get started...you've been very patient.
CBD and serotonin for depression
Remember, the major class of antidepressants on the market revolves around boosting serotonin.
This may only work for about 30% of the patients but it's clearly in play.
The problem is that the brain doesn't like this artificial interference and will start to suppress natural serotonin function (called tolerance).
This leads to the constant merry-go-round of different medications or doses will all lead to the same fate.
What about CBD and serotonin for depression?
This may be one of its most powerful effects.
First researchers wanted to see if serotonin was a basis for CBD's antidepressant effects.
They used a chemical to block serotonin function and the antidepressant effects went away:
However, only PCPA treatment abolished CBD-induced behavioral effects in FST, indicating the participation of serotonergic mechanisms.
https://www.ncbi.nlm.nih.gov/pubmed/29885468
They compared it with Prozac and both functioned in the serotonin pathway.
Remember though that SSRIs like Prozac only move serotonin in one direction...up!
What about CBD...can you get serotonin syndrome from CBD? (see CBD and serotonin syndrome).
Another study looked at CBD's effect in the serotonin pathway after causing an injury:
Seven days of treatment with CBD reduced mechanical allodynia, decreased anxiety-like behavior, and normalized 5-HT activity.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6319597/
The pain threshold is highly tuned by serotonin so when it runs low, we feel more pain.
The keyword there is "normalized". 5HT is short for serotonin.
This is really important! Throughout the research, we see words like "normalize", "modulate", and "rescue".
Not increase or reduce.
This gets to the beauty of CBD.
It appears to act as a feedback system on these pathways. A constraint.
Cancer is a perfect example of this multi-phasic effect:
- Healthy cell, low inflammation - CBD has no effect
- Healthy cell, high inflammation - CBD reduces inflammation
- Cancerous or virally infected cell - CBD INCREASES inflammation
Three different effects for three different situations.
How does CBD do this?
For serotonin, CBD is called an allosteric modulator.
The chart of CBD's pathways is here.

https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5345356/table/T1/
What does that mean?
Usually, a chemical is an agonist (boost), the antagonist (reduce), or inhibitor (block).
For example, THC boosts CB1 activity which is partially why it's psychoactive (and builds tolerance).
CBD acts as a feedback from the receiving neuron to the sending neuron.
- "We're all full here...stop sending"
- "We're running low, send some more"
- "We're just about fine...nothing needed"
The negative reverse modulator is the technical term.
One final study for CBD and serotonin as it wraps this all up in a bow:
In vivo microdialysis revealed that the administration of CBD significantly enhanced serotonin and glutamate levels in vmPFCx in a different manner depending on the emotional state and the duration of the treatment.
https://www.ncbi.nlm.nih.gov/pubmed/26711860
Okay...we have our two big players, serotonin and glutamate. The PFC is the prefrontal cortex, our rational guard against our most animal instincts.
The fascinating part is the last section…" different manner depending on emotional state".
If you keep ramping up serotonin, you get very nasty effects and even dangerous or deadly results (serotonin syndrome).
We'll leave the homicidal and suicidal thoughts to this review here.
CBD has not been shown to cause serotonin syndrome even at doses up to 1500 mg which is fascinating and we don't have a documented overdose.
Check out CBD and serotonin pathways if you really want to get deep into this powerful manager of mood.
Glutamate was mentioned as well in that last study. Let's go there now.
CBD and glutamate/GABA for depression
As we mentioned, glutamate is the new kid on the block for depression.
Both too low in certain areas (prefrontal cortex) or too high in others (neurotoxic effects).
What about CBD and glutamate/GABA balance?
We've spent a lot of time on GABA due to anxiety (GABA is the main pathway for benzos).
When they blocked the serotonin effects of CBD, the glutamate boost also went away.
That's because serotonin manages glutamate and GABA:
In several brain regions, 5-HT is diffusely released by volume transmission and behaves as a neuromodulator rather than as a “classical” neurotransmitter.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430669/
Glutamate and GABA are two such players under its control.
We saw how CBD helps reign in serotonin function above.
A study on CBD and autism (which can show glutamate imbalance specific to brain areas) looked at CBD's effect on glutamate/GABA balance.
Their findings:
CBD increased subcortical, but decreased cortical, Glx. Across regions, CBD increased GABA+ in controls, but decreased GABA+ in ASD; the group difference in change in GABA + in the DMPFC was significant.
https://www.nature.com/articles/s41386-019-0333-8
This is interesting since CBD had different effects on glutamate/GABA balance depending on the setting (Autism being the 2nd state).
Low glutamate in the prefrontal cortex is thought to be part of why there can be mental and social deficits with autism.
CBD actually lowered GABA (the opposing force to glutamate) in that brain area but for the autistic group!
The key to glutamate and GABA is balance. This is a great clue for CBD's effects considering the two extremes of glutamate activity at the NMDA receptor:
The glutamate NMDAR is implicated in certain neurological disorders and whilst psychosis/schizophrenia concurs with reduced NMDAR activity, these receptors are hyperactive in convulsive disorders like epilepsy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342457/
CBD's original claim to fame was for epilepsy (in fact, there's an FDA approved CBD drug for that).
The newer studies on CBD and schizophrenia are fascinating.
So..CBD is showing positive effects for both the extremes:
- Too much glutamate - seizures
- Too little glutamate (by brain area to make it more confusing) - schizophrenia
The whole glutamate framework that's emerging is so important that we have a full review of CBD and glutamate for mental health.
Let's move on to neurogenesis.
CBD and neurogenesis for depression
If you've noticed, serotonin and glutamate were intertwined. The same goes for neurogenesis.
Serotonin is a major manager of BDNF, our brain's fertilizer. We also saw how CBD supported serotonin function directly so we would expect to see the knock-on effect for neurogenesis.
Do we?
A groundbreaking study found that antidepressants like SSRI's lost their punch when neurogenesis was blocked:
Chronic treatment with fluoxetine and imipramine induced anxiolytic-like effects in the novelty suppressed feeding test in control mice but not in animals that were submitted to x-ray-irradiation of the SGZ (SGZ-x-irradiation), a procedure that blunts neurogenesis by killing cells undergoing proliferation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648779/
And CBD's effect:
A study conducted with transgenic mice (GFAP-TK mice) showed that the anxiolytic effect of chronic CBD administration (14 days) in stressed mice depends on its proneurogenic action in the adult hippocampus by facilitating endocannabinoid-mediated signaling.
Same effect!
To cut to the chase:
Preclinical studies have shown CBD to induce synaptic plasticity and facilitate hippocampal neurogenesis,29,30 with some evidence suggesting that the proneurogenic action of CBD via the hippocampus may underlie its anxiolytic effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5908414/
Check out CBD and neurogenesis or CBD and BDNF for full reviews of these effects.
This is the repair side. Can we also address the ongoing damage (immune response, chronic stress, etc)?
CBD and stress and inflammation response for depression
We have two powerful systems at work here...hormones and immune responders.
Let's start with the hormone stress responses.
Serotonin is one of our primary managers of the stress response. It's the general so to speak.
One of it's enlisted weapons is actually an endocannabinoid called Anandamide.
Anandamide is named after the Hindu goddess of bliss, Anand.
Prefrontal Cortical Anandamide Signaling Coordinates Coping Responses to Stress Through a Serotonergic Pathway.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3366159/
Goodness...it all comes back around. Serotonin is in play.
What does CBD do for anandamide? It works against the chemical that breaks down anandamide called FAAH.
CBD also inhibits FAAH, which results in increased anandamide levels.
https://www.frontiersin.org/articles/10.3389/fphar.2018.00482/full
Check out the woman who can't feel pain, depression, or anxiety because of a missing FAAH gene.
We'll take a little of that, please. Just a little.
Anandamide is the main throttle for CB1 activity who's the primary function to slow...things...down.
That's the glutamate angle and in our view, is why people chronically use THC (not to get high) which fills in nicely for anandamide.
Of course, THC has some issues (normalization, addiction, reductions in brain matter in certain areas, etc). See CBD versus THC or why you must use CBD if you smoke cannabis.
Then there's the whole hormone angle and front and center is cortisol..our primary stress hormone.
Look what happens when they block CB1 activity:
pharmacological blockade of the CB1 receptor in humans may directly increase cortisol levels, supporting the hypothesis that, similar to rodents, eCB signaling constrains activation of the HPA axis in humans.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677118/
So less activity where CBD works means more stress hormone.
A study on CBD for sleep and anxiety showed a direct effect:
Another crossover study showed that plasma cortisol levels decreased more significantly when given oral CBD, 300 to 600 mg.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6326553/
Check out CBD and cortisol here.
What about the hormone that starts the whole stress response rolling (downhill if we may add)?
After all, this little beauty is why SSRI antidepressants can actually INCREASE anxiety and depression in the first few weeks until the neurogenesis kicks in.
CRF (corticotropin releasing factor).
Like we said, just boosting serotonin in one direction is a tricky proposition since it has its hands in so many pies.
As for CBD and CRF:
Interestingly, cannabidiol at low (5 mg/kg) and intermediate doses (15 mg/kg) successfully blocked the effects induced by acute stress on corticotropin-releasing factor, pro-opiomelanocortin, and glucocorticoid receptor gene expression.
https://journals.sagepub.com/doi/abs/10.1177/0269881118805495?journalCode=jopa
Just to recap...chronic stress causes damages to key areas of the brain that are implicated in depression.
What about the hyperactive immune response?
This is the link to early infection or trauma and depression...even auto-immune!
CBD at its core is a powerful anti-inflammatory throughout the body and nervous system.
Microglia, the immune system's primary generals in the nervous system are showing up across a range of mental health issues including depression.
Hyperactivation!
A study on Alzheimer's looked at CBD's multifaceted effects:
In summary, CBD is able to modulate microglial cell function in vitro and induce beneficial effects in an in vivo model of AD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3102548/
And the little henchmen of the immune response to inflammation...cytokines?
From a study of asthma (an inflammatory disease at its heart):
The levels of IL-4, IL-5, IL-13, IL-6, IL-10, and TNF-α were determinate in the serum. CBD treatment was able to decrease the serum levels of all analyzed cytokines except for IL-10 levels.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458548/
By the way, IL-10 is the lone anti-inflammatory agent on that list. It's a lonely place.
The net net...too much inflammatory response is toxic to the brain.
Retrenchment and actual brain loss can result.
Check out CBD and neuroinflammation to really get into the weeds of it.
So...we spend a great deal of time looking at the pathways because it's important to make sure there's actual research backing something.
On to the studies of CBD and depression.
CBD studies on depression
Interestingly, we have more studies on CBD and anxiety than for depression.
Most of the studies to date are animal studies are studies on specific pathways that we covered above.
One study looked at mice specifically bred to display depressive-like symptoms.
They are then placed in a forced swimming tank and when they stop swimming, that's called immobility.
Depression will lead to this state faster.
It's a standard test for antidepressants in animal studies and they delay this immobility.
CBD had the same effect!
The conclusion was that the effects of treatment with cannabidiol were fast-acting and sustained, persisting for up to seven days after a single dose was administered to animals belonging to different models of depression (including a stress model and a genetic susceptibility model).
https://neurosciencenews.com/cbd-depression-9775/
Interestingly, they look at brain structure after the experiment and found the tell-tale signs we've discussed ad nauseum above:
When we studied the mechanisms involved in these effects, we found that treatment with cannabidiol induces a rapid rise in levels of brain-derived neurotrophic factor, or BDNF.
And in the critical area that's susceptible to all the insults we discussed above (stress, inflammation, chemicals, etc):
We also observed an increase in synaptogenesis in the prefrontal cortex of these animals.
We expect this after everything we've looked at but it's nice to see it in living creatures.
Human trials on CBD and depression are ongoing and planned and we'll make sure to add them here as they come online.
Let's look at other tools we found along the way in this research.
Other tools for depression
There are some interesting players out there for depression which were so intriguing, we did full reviews on them:
- Psilocybin - active ingredient in magic mushrooms will be a game-changer for depression within a few years
- NAC N-acetylcysteine - turns out it might be a huge supporter of glutamate balance
- Mindful meditation - slow-motion neurogenesis
- Exercise - anti-inflammatory and booster of neurogenesis
Check out the full reviews.
Psilocybin isn't legal yet (except for a small and growing list of places).
NAC is cheap, safe, and available right now. It can take weeks to really kick in but the research is very interesting (also for addiction).
Mindful meditation and exercise are no brainers. The Calm app is a great way to get started for beginners. As for exercise, at least 30 minutes a day.
Check out CBD, exercise, and mindful meditation for the research on brain growth!
Some practical questions on CBD itself.
How much CBD to take for depression
We actually have some guidance on this.
Some of the studies were up to 600 mg/day but the key is neurogenesis (the basis for SSRIs and CBD after all).
Neurogenesis effects were shown to peak at 300 mg of CBD/day. That effect actually starts to go down from 300 to 600 mg.
Short term, higher doses might bring relief but longer-term, 300 mg is the ideal max dosage.
This may be a lower amount for a given person depending on weight, liver function, genetics, etc.
The dosage can be broken up into separate doses totaling 300 for the day.
Try to take after meals and hold under tongue up to 60 seconds to maximize bioavailability.
Work with your doctor or naturopath with any supplement.
What about the type of CBD?
What's the best CBD for depression
There are basic requirements for any legitimate CBD:
- Organically grown in the US at an FDA registered farm
- CO2 processed
- 3rd party tested
- No THC (THC actually has been shown to increase long term risk of depression)
- No pesticides
- No solvents
- No heavy metals
- No bacteria
- No mold
Those are the basics and we meet all of these. We actually test twice since our whole family uses IndigoNaturals.
Then there's the question of CBD isolate versus Full spectrum.
All the research listed above (in fact, over 100's of studies we reference on our site) is based on CBD isolate. CBD by itself.
Learn all about CBD isolate versus full spectrum.
The big issue there is a histamine response (allergy pathway).
We see lots of people who have bad responses to full-spectrum which go away with CBD isolate.
That's why we started IndigoNaturals, to begin with.
Here's the deal…
40-60% of people have histamine issues and that number goes up as we get older and for women
Histamine is part of the immune response so more effect there goes against what we've learned above.
For this reason, we want the cleanest CBD we can get.
All the plant material in the full spectrum is not the right direction and there's no research to back it.
Afterall, allergic reactions are inflammatory in nature (remember the study on asthma??).
If you've stuck with us this far, congratulations.
A big part of addressing any mental health issue like depression is to unravel and deconstruct it.
You can then target the pathways directly (inflammation, neurogenesis, stress response, etc).
The neurogenesis piece is really the key. Glutamate balance is the new kid on the depression block.
CBD and NAC together may be powerful allies against depression. Keep us posted and be well!
Don't forget steroidal hormones (get tested) and Vitamin D.
Related Research:
CBD versus SSRIs
Tips to taper SSRIs
Edit your mental health code
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.