Research on Glutamate and Mental Health - CBD and NAC

For a few decades now, serotonin has gained all the fame.
The so-called "feel good" neurotransmitter.
That's a bit of a misnomer as it's involved in ALL human behavior but we'll leave that to our review on serotonin here.
Then came dopamine and the reward circuit...key to mental health and addiction.
Very powerful but also nearly impossible to directly impact with medication without blowing out some other system. Again, they're all intertwined.
GABA preceded these mainly due to the discovery of benzos (see CBD versus benzos) and their explosion in use (and addiction).
We've covered all of these in detail but our big review of NAC (N-acetylcysteine) and mental health really grabbed our attention.
Towards Glutamate...the workhorse of brain activity.
The other neurotransmitters are managers or modulators of various pathways.
Glutamate carries out the actual orders though as we'll see below.
More importantly, new research is pointing to glutamate across almost every mental health issue and addiction (see CBD and addiction).
Interestingly, there are ways to help balance this primary workhorse of the brain (CBD and NAC).
This all started with questions on why people chronically use THC (cannabis) for us and the answer we found was fascinating.
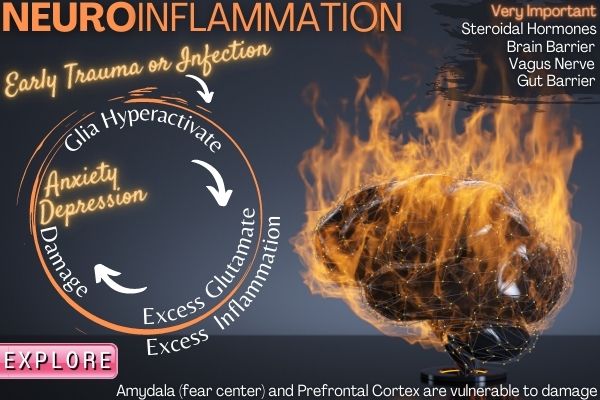
The newest and most powerful research on mental health centers around how early trauma, infection, and stress cause life-long changes (more here).
Glutamate may be the assasin behind all this damage! More below..especially how to counter this.
And the endocannabinoid system where CBD works may be the linchpin:
In this biological context, endocannabinoids are released to retain NMDAR activity within physiological limits.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342457/
Goodness. "within physiological limits". balanced!
We'll cover these topics:
What is glutamate and how does it work in the brain
The glutamate and glutathione connection
Glutamate and GABA complicated relationship
Glutamate and Anandamide (the THC connection)
Glutamate and neurogenesis (player behind the curtain)
Glutamate imbalance and mental health issues
Glutamate and depression
Glutamate and anxiety
Glutamate and schizophrenia
Glutamate and OCD
Glutamate and addiction
Are there ways to balance glutamate activity
CBD and glutamate
NAC and glutamate
How much CBD and NAC for glutamate balancing
The best CBD and NAC for glutamate balancing
Let's get started. Of the 100's of reviews, we've done with nearly 1 million words across dozens of NIH studies…
This one may be the most important!
What is glutamate and how does it work in the brain
Technically, glutamate is an amino acid that we mainly (multiple sources since it's so important) get from glutamine which is wildly available in our food. It can also be made within our nervous systems via different pathways and the glial cells have a big role there.
Glial cells are immune system commanders so that's an interesting connection with mental health following infection, trauma, injury, etc that we'll discuss below.
Simply put, glutamate is the "gas pedal" of the brain and body.
It increases activity both within neurons and between them.
It's the main excitatory neurotransmitter and makes up the vast majority of brain activity.
Glutamate is everywhere in the brain and body!
It is used by every major excitatory function in the vertebrate brain, accounting in total for well over 90% of the synaptic connections in the human brain.
https://en.wikipedia.org/wiki/Glutamate_(neurotransmitter)
What most people don't realize is that you have specific neurons for dopamine and serotonin generation and function.
You need glutamate to activate those and every other neurotransmitter-specific neuron!
All roads lead back to Rome and glutamate may be the capital city.
For this reason, glutamate balance is key to a healthy functioning brain.
Part of this balancing system is the entire detox system called glutathione.
Let's go there now.
The glutamate and glutathione connection
Glutathione is our main anti-inflammatory pathway.
We covered it in detail at our CBD and glutathione or CBD and oxidative stress reviews.
It has a fascinating second job in regards to glutamate.
To understand why, we have to see what makes up glutathione.
It's composed of three amino acids:
- Cysteine
- Glycine
- Glutamate
Glutamate is readily available as we discussed above. Glycine is also pretty abundant.
The real rate limiter of glutathione production is cysteine which is why NAC is so valuable!
NAC (N-acetylcysteine) is a donor of cysteine.
Besides its very important role in sponging up free radicals, glutathione is also a temporary storage for excess glutamate.
Put another way, if we're low on cysteine (more likely) or glycine, glutamate is free to run amok if levels are too high.
Glutathione sponges up excess glutamate.
Why is excess glutathione an issue?
Just this:
Excess extracellular glutamate may lead to excitotoxicity in vitro and in vivo in acute insults like ischemic stroke via the overactivation of ionotropic glutamate receptors.
https://www.frontiersin.org/articles/10.3389/fnins.2015.00469/full
That's a one-time big pop of glutamate (like with a stroke).
What about chronic glutamate excess?
It is involved in the neuro-circuitry of memory, emotions, and cognition and is implicated in myriad psychiatric conditions, including depression, anxiety, schizophrenia, drug addiction, and neuropsychiatric disorders.
https://www.psychiatrictimes.com/bipolar-disorder/glutamate-and-psychiatry-2012-and-away
Okay...so all of mental health.
There are tell-tale signs of reduced glutathione via increased oxidative stress across multiple mental health issues:
Accruing data suggest that oxidative stress may be a factor underlying the pathophysiology of bipolar disorder (BD), major depressive disorder (MDD), and schizophrenia (SCZ).
When these researchers looked closer:
We found that the levels of reduced, oxidized, and total GSH was significantly decreased in all psychiatric conditions compared to the control group.
https://academic.oup.com/ijnp/article/14/1/123/657694
GSH is glutathione!
Interesting...glutathione, our primary anti-oxidant and a sink for glutamate were depleted.
Check out CBD and neuroinflammation for more detail.
We'll look more at boosting glutathione (a good thing anyway) below in the NAC section.
So...what's the opposing force to glutamate in the brain?
Glutamate and GABA complicated relationship
If glutamate is the gas pedal, GABA is the brake pedal in the brain.
We've covered it in detail (CBD and GABA, CBD versus benzos for GABA) in our whole review of anxiety.
Afterall, benzos (the leading medication for anxiety) pump up GABA...until they don't (tolerance and addiction).
Here's the fascinating piece.
GABA comes from glutamate!
That's right...there are mechanisms to track the balance between these two and convert glutamate into GABA as needed.
For example, when it's time to sleep (see CBD and sleep).
There's a great deal of focus on boosting GABA for anxiety, OCD, etc but you have to look at the two in conjunction.
If you boost GABA (such as with benzos), the brain will push the other way and actually reduce naturally-occurring GABA function. Glutamate actually ramps up over time!
Our review of CBD and GABA dive into this process.
That's why some people who stop long-term benzo use can actually experience seizures (excess glutamate)!
Check out CBD to wean off benzos.
Again, GABA function has been the main focus but new research is pointing to glutamate as a key player...maybe THE key player.
Let's look at that now at the aspect that caught our attention. We'll set the stage.
Glutamate and Anandamide (the THC connection)
We know someone that smokes cannabis daily. Multiple times a day.
We asked them why they did it and this was the answer.
"It slows things down. Otherwise, I have a constant stream of thoughts, negative thoughts, doubts, etc."
They weren't using cannabis for a high per se. They were self-medicating to slow things down.
Hmmm...that's an excess glutamate function.
What on earth would THC (the main active ingredient in cannabis) do there? Specifically.
THC fills in nicely for our naturally occurring endocannabinoid in the brain called Anandamide.
Anandamide is named after the Hindu goddess of bliss so you can guess the effect.
It wears many hats but a big role is as a stress response reservoir.
When things get stretched, Anandamide calms things down.
What's the connection with glutamate though?
As part of calming things down, you can guess the effect on our major excitatory neurotransmitter:
Anandamide, THC, and other anandamide-receptor agonists inhibit the presynaptic release of the excitatory neurotransmitter glutamate in the hippocampus (Shen et al. 1996).
https://www.sciencedirect.com/topics/neuroscience/anandamide
What Anandamide and THC have in common is that they both boost CB1 (our main endocannabinoid receptor in the nervous system).
CB1 activity (agonist) slows...things….down.
No wonder people are using THC. The issue is that THC hits the receptors too strongly (compared to natural anandamide) and the brain counters this effect long term.
That's tolerance!
You end up with lower CB1 function long term unless you're constantly pumping THC (which just makes the future situation worse).
There's been a long-running debate on whether there's a risk for THC use and schizophrenia or that people with risk of schizophrenia are self-medicating a shared pathway with THC.
Before we jump into mental health issues, let's look at one last, very important piece.
This is the future of mental health and explains much of what actually works these days.
Glutamate and neurogenesis (player behind the curtain)
Neurogenesis is the ability to build not only more neurons but more connections between them.
A re-integration of brain stuff if you will.
In our CBD and depression review, we described how new research is coalescing around the view that its core driver is a retrenchment in the brain.
Loss of connections, nodes, and communication across the brain.
We need to look no further than to new substances that have fascinating, powerful, and long term effects on a range of mental health issues.
What do SSRIs (the old guard), psilocybin, ketamine, NAC, and CBD all have in common?
A boost to neurogenesis and synaptic plasticity!
They may activate this via the serotonin pathways of further downstream to BDNF itself.
See CBD and serotonin or CBD and BDNF to understand those players.
As research is finding:
Several lines of evidence suggest that adult neurogenesis, the production of new neurons in adulthood, may play a role in psychiatric disorders, including depression, anxiety, and schizophrenia.
https://www.ncbi.nlm.nih.gov/pubmed/25178407
Where does glutamate fit in here?
You can think of glutamate at the Roman emperor with his thumb up/thumb down decision on a gladiator's fate.
Glutamate levels literally decide whether a neuron or connections survives or dies:
To support this, studies indicate that the blockade of NMDAR function leads to neuronal apoptosis and degeneration
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5791143/
Apoptosis is cell-programmed death. It just happens to be under the control of the endocannabinoid system (we'll discuss later).
If we zoom out, glutamate also affects macro-level brain architecture.
Two very important ways.
First, too much glutamate is toxic to the very architecture of the brain.
This can exhaust the repair/rebuild function of the brain (neurogenesis) and lead to an actual loss in connections and function.
For example, if you burn out (essentially what too much glutamate does) serotonin pathway neurons, you may get reduce function.
The hippocampus is especially vulnerable to damage from stress, injury, infection, and drugs.
Interestingly, our bodies' response to all of those involves the immune system's inflammatory response.
Hence the ties with early infection and trauma (even in-utero) for mental health later on.
The immune response is primed to respond too aggressively and glutamate is primarily created and managed by our immune cells in the brain (microglia and astrocytes).
Ah-ha! There's that connection. Please read that back over again. It's the most important piece as our brain immune cells just leak out excess glutamate when ramped up!
That's the insulting side...too much glutamate causes brain loss.
On the flip side, glutamate is intimately tied in with the process of neurogenesis itself so if it's too low, we can grow/repair.
Glutamate receptors, AMPA, kainate and NMDA have also being recognized as crucial players at later stages of neurogenesis and have been clearly identified as critical elements of neuronal plasticity in newly born neurons in the adult brain
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2538920/
AMPA, kainate, and NMDA are the three main receptors for glutamate.
GABA is also involved in the process and we've shown how it's derived from and opposed to glutamate.
They shape the process of landscaping our brains!
The goal though is homeostasis... the balance of glutamate is critical.
If you need a good example of glutamate's effect, just look at the ultimate dynamic system of plasticity..memory.
Each time a memory is formed, new connections have to be made. Fast and pretty stable considering.
You're doing that by the second. Some will wither away as you'll never strengthen them again (hopefully not this article).
Others will stay with you for the rest of your life.
Glutamate is front and center in this process:
In experiments with rats, the UH team found that glutamate transport molecules increased by more than 100 percent in a region of the brain called the hippocampus 30 minutes after the onset of long-term potentiation – the memory-forming process.
https://www.sciencedaily.com/releases/2002/03/020313075047.htm
Memory is the most robust example of neurogenesis and glutamate is the gas for BDNF, PSD95, and other builders.
Again, we have very complex systems to make sure it doesn't get too low or too high.
What happens if they fail?
Glutamate imbalance and mental health issues
Let's look at both extremes in the context of mental health and we'll look at the "manager" of cop on the beat for glutamate levels.
- Too much glutamate - neurotoxic effects
- Too little glutamate - brain withering effects
We'll start with too much.
We're seeing examples across the board:
For instance, an elevated level of glutamate was identified in the postmortem frontal cortex of patients with MDD or BD
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984954/
MDD is short for major depression and BD is short for bi-polar disorder.
Think of the mental health issues where there's an excess of activity:
- OCD - excessive, repetitive thoughts
- ADHD - excessive mental activity
- Anxiety - hyperactive amygdala (fear and emotional processing center)
- Bi-polar - manic phase
Some of these are expressions of hyperactivation in certain brain areas.
Then there's the damage done by excess glutamate.
This is showing in diseases such as schizophrenia and depression.
What about lower amounts of glutamate activity?
Depression is a big clue here.
Depending on the brain area, schizophrenia and other mood disorders also figure in.
For example, depressed activity in the prefrontal cortex (our rational brain) has been linked with schizophrenia (the so-called negative symptoms).
Many mental illnesses creep up during puberty. What's the connection there?
It's a period of intense brain remodeling (see CBD and teen anxiety or CBD and child anxiety).
That's code for neurogenesis and glutamate is front and center.
Before we jump into each mental health specifically, let's look at what governs this balance.
Two key systems:
- Astrocytes and microglia (immune cells)
- Endocannabinoid system (ah-ha!)
First, astrocytes and microglia.
Thus, there exists a tight coupling between the glutamatergic system and brain energy metabolism via astrocytic functions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984954/
The "tonic" or baseline glutamate is managed by astrocytes.
It is thus of particular interest that astrocytic abnormalities are continuously implicated in human and animal studies of mood disorders, although changes in other kinds of glial cells have also been noticed
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984954/
What's causing this loss of glial cell function (including astrocytes)?
As stress may incur an excess of glucocorticoids or reductions in neurotrophin levels which are thought to be associated with decreased astrocytic density and impaired astrocytic function, it may, in turn, lead to disruption of glutamatergic system and subsequent neurotoxicity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984954/
The insults: Infection, chronic stress, trauma, drugs, etc.
We covered this in detail at our CBD and depression, CBD and anxiety, or CBD and neuroinflammation reviews.
As we get closer to CBD, let's look at the endocannabinoid system.
The endocannabinoid system is a key "balancing" manager of other systems:
- Nervous system - neurotransmitters such as glutamate, GABA, and serotonin
- Endocrine system - stress hormones and others
- Immune system - inflammatory processes including microglia and astrocytes!
Goodness...so the intersection of everything we're talking about.
People...this may be the weak link in glutamate balancing:
In this biological context, endocannabinoids are released to retain NMDAR activity within physiological limits.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342457/
We're dropping the mic right now!
"within physiological limits". Based on everything we've discussed, these are three most important words in this review.
NMDA is the key glutamate receptor that's attracting so much attention for mental health issues.
Of these, the NMDARs have received much attention because their deregulation is observed in many neurological disorders, such as neurodegenerative diseases [12], neuropathic pain [13, 14], mood disorders and psychosis-schizophrenia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342457/
"To retain NMDAR activity within physiological limits".
To confine it to a range!
Goodness… this is what we're looking for.
Okay...enough already. Let's look at some core mental health issues and glutamate function.
Stick with us...the payoff at the end to review new substances that are showing profound effects on these issues via the glutamate pathway.
Glutamate and depression
On the surface, this would appear to be a case of hypofunction or too little glutamate.
It is (on the surface).
We'll dig deeper to see what comes first...the chicken (too little function) or the egg (brain's response to excess glutamate prior)!
We have to lead this section with ketamine.
There are drawbacks to ketamine (tolerance) but its effect on treatment-resistant major depression is an important clue.
It can have profound effects on depression very quickly. How is this possible?
There's a great explanation here:
https://www.nih.gov/news-events/nih-research-matters/how-ketamine-relieves-symptoms-depression
Essentially, ketamine was able to spur the growth of the spines that come off neuronal connections called dendrites.
Think of the little branches from a tree trunk. So...neurogenesis.
Chronic stress causes these dendrites to retreat and if this happens in the prefrontal cortex, depression is the net result.
We spoke of the "insults" above such as stress. This experiment shows how this works:
Further experiments showed that the newly formed spines were crucial for sustained reversal of the negative effects of stress. When the ketamine-induced spines were eliminated, the mice again showed depression-like behaviors.
So how does it drive this connectivity?
Glutamate. Specifically, it slows down activity at the NMDA receptor, one of the three glutamate receptors.
That is its main mechanism of action.
In the first 20 min post-infusion, ketamine-induced a rapid increase in 13C-glutamine enrichment, indicating an acute surge in prefrontal glutamate-glutamine cycling
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6098048/
This is very interesting. Essentially, it's boosting glutamine which is in a constant dance back and forth with glutamate (they cycle back and forth).
It's giving the brain a brake from too much glutamate!
And guess who's in charge of the dance?
There is robust evidence that astrocyte and satellite oligodendrocyte populations are reduced in the prefrontal cortex and other cortical regions in post-mortem tissue from individuals who had suffered from major depression (94) and bipolar disorder (95),
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3671489/
Astrocytes. Immune system again. It turns out they are intimately involved in the cycling or maintenance of glutamate throughout our nervous system.
We're moving away from our neuron-centric view of mental health to focus more on the immune agents like astrocytes and glial cells:
The glutamate/GABA–glutamine cycle is a metabolic pathway that describes the release of glutamate or GABA from neurons which are then taken up into astrocytes (star-shaped glial cells). In return, astrocytes release glutamine to be taken up into neurons for use as a precursor to the synthesis of glutamate or GABA.
https://en.wikipedia.org/wiki/Glutamate%E2%80%93glutamine_cycle
But wait a minute...ketamine REDUCES glutamate activity at the NMDA receptor.
What gives?
So a recap…
- Stress, trauma, infection, genetics can cause damage via excessive glutamate especially to the astrocytes
- Astrocytes can't keep up their bargain in the glutamate/glutamine cycling
- Ketamine recalibrates the cycling (more glutamine...the product from astrocytes!)
- Synaptic growth results
This may sound counterintuitive...block activity to refresh the pathway but we see it all over the body.
We covered it in detail at our CBD and tolerance review.
When there's excessive anything in a given pathway (especially something as toxic as glutamate), the brain responds by reducing sensitivity and/or # of receptors.
It's a self-protecting mechanism.
- SSRI's do it with serotonin (See CBD and serotonin)
- Benzos do it with GABA (see CBD and GABA)
- Nicotine and acetylcholine
- THC and anandamide
It's why ketamine is showing promise for peripheral nerve pain which can result from too much glutamate.
- Give the system a break so it can normalize!
- We could go on and on...islet cells and diabetes. THC and CB1 receptors.
Interestingly, glutamate is the key trigger that almost every cell uses to fire...or fire too strongly!
As for depression specifically…
In addition, the discovery that antagonists of the N-methyl-D-aspartate (NMDA) receptor, notably ketamine, produce rapid improvement in depressive symptoms (within hours), even in TRD patients, has shifted efforts towards novel agents targeting the glutamatergic system
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4803609/
This is the future folks. Keep in mind that there are no good treatments for major depression before this came along (except for psilocybin...an explosion in neurogenesis and retooling of...the immune system).
Especially the treatment-resistant kind.
To have any effect much less fast-acting effects are promising.
We'll do a whole review on CBD, glutamate, and depression where we really get into it.
Next, up let's look at huge morbidity and potential cause of depression….anxiety.
Glutamate and anxiety.
The two go hand in hand, unfortunately.
The risk of getting one if you have the other is very high:
The prevalence of comorbid anxiety disorder and major depressive disorder (MDD) is frequent and perhaps as high as 60%.
https://www.psychiatrictimes.com/understanding-comorbid-depression-and-anxiety
That's the baseline...it can actually go higher.
What in the world is going on...what's the connection for two seemingly opposite effects (feel too much...don't feel enough).
Glutamate.
We spend the better part of a year investigating all aspects of CBD and anxiety.
There's a general explanation in research and the medical world that anxiety is a product of reduced GABA.
That's definitely a factor as we covered in CBD and the mechanism of anxiety.
However, after reading above, we now know that all GABA is made for glutamate!
In fact, that's the only way it's made.
It goes deeper than that.
Think of anxiety as a state of nervous system stress. In fact, you can get anxiety from histamine response (which is why anti-histamines can reduce anxiety), oxidative stress (see CBD and oxidative stress), and host of issues.
More important, anxiety shares the same risk factors as depression:
- Early trauma
- Social rejection
- Early infection
- Lack of neurogenesis
The primary hammer that medicine uses for anxiety is benzos.
Their action is simple...boost the GABA pathway (with some nasty side effects)
But if we're talking about GABA, we're ultimately talking about glutamate...the other side of the coin.
You can't really separate them.
Back out our original point...chronic anxiety can and will probably lead to depression.
Stress chemicals (cortisol, etc) spike glutamate. Excessive and chronic glutamate is toxic especially in the hippocampus and prefrontal cortex.
It's a nasty slippery slope.
Back to anxiety specifically.
The newer research is really looking at the glutamate side of things now:
A growing body of evidence suggests that glutamatergic neurotransmission may be involved in the biological mechanisms underlying stress response and anxiety-related disorders.
https://www.sciencedirect.com/science/article/pii/S0091305711001201?via%3Dihub
Aside from just eating up GABA, our calming neurotransmitter, it goes deeper.
Right to the heart of emotional memory.
Remember how glutamate bursts are key to creating and maintaining memories?
The glutamatergic system mediates the acquisition and extinction of fear-conditioning.
https://www.sciencedirect.com/science/article/pii/S0091305711001201?via%3Dihub
Think of fear-conditioning as a type of learning...albeit a bad one (just like addiction - see CBD and addiction).
The more these anxiety and fear circuits fire, the stronger they become.
Like water flowing downhill.
Glutamate is key to this firing and marbling of anxiety responses.
In fact, the same NDMA blockers (like ketamine and a range of others) have shown anti-anxiety effects as well.
Other substances have also shown positive effects and just guess where they operate:
This could mainly be attributed to their ability to modulate ionotropic glutamate receptors, especially NR2B subunits.
https://www.sciencedirect.com/science/article/pii/S0091305711001201?via%3Dihub
Not GABA but glutamate.
Perhaps we've been looking in the wrong place?
A study looked at brain scans directly for social anxiety:
For SAD subjects, there were significantly higher whole brain levels of glutamate and glutamine, though no significant differences in GABA.
https://www.ncbi.nlm.nih.gov/pubmed/18206286
This is interesting because GABA has been the focus till now (primarily due to benzo popularity and effects).
For anxiety, we have to understand that stress, in its various forms (chronic, traumatic, immune-related, etc) release glutamate.
This makes sense if you think about what anxiety is really there for.
Anxiety is a response to make you do something! NOW!
Stop doing something harmful or react quickly to something harmful.
Glutamate is the engine behind focus, action, and engagement.
Data from early studies suggest that chronic stress causes prolonged periods of stimulated glutamate release following acute stress exposure, at least in the hippocampus
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3645314/
That review is a great review of how stress hormones (like cortisol) and glutamate are toxic to the brain when exposed long term.
As we saw with depression, this elevated glutamate has an end-game:
Recent studies have found dendritic remodeling, synaptic spine reductions, glial loss, and possibly volumetric reductions from glutamate excess following stress.
https://www.psychiatrictimes.com/bipolar-disorder/glutamate-and-psychiatry-2012-and-away
Loss of neurogenesis especially in the prefrontal cortex which is the rational player in the anxiety circuit to keep the amygdala (emotional/fear center) in check.
Let's move on to schizophrenia.
Glutamate and Schizophrenia
This is the big one.
We've covered CBD and schizophrenia and even NAC and schizophrenia since their effects were very interesting on a seemingly intractable disease.
The focus was on dopamine for decades but lately, there's a shift and you can guess where to.
Again, ketamine and PCP (another NDMA affecting drug) were integral to this shift as they can actually mimic schizophrenia symptoms at certain doses.
The second clue was the fact that glutamate receptors are really dense in dopamine-centric areas tied to schizophrenia (so dopamine was a knock-on effect).
Finally, a glutamate receptor gene variant is highly linked with schizophrenia rink.
In fact, high doses of stimulants (hello glutamate) can look just like schizophrenia:
Consistent with the antipsychotic effects of depleting dopamine, high doses of stimulants induce a psychosis that clinically resembles the acute phase of paranoid schizophrenia
https://onlinelibrary.wiley.com/doi/10.1111/pcn.12823
All this speaks to excess glutamate. Huge spikes in glutamate.
Interestingly, research is pointing to hypofunction (reduced) at the NMDA receptor in the prefrontal cortex.
Why would we see reduced receptor activity if there are elevated glutamate levels?
This goes back to the tolerance mechanism we looked at above with depression.
The brain will try to compensate when a critical chemical is too high or too low for long periods of time.
If there's too much glutamate? Reduce the receptor sensitivity and/or numbers to compensate.
This is where it can get complicated. You can have NMDA receptors on inhibitory neurons!
For example, you have glutamate inputs on neurons that drive GABA (or other braking pathways) neurons!
From research on schizophrenia:
One proposed cause of reduced inhibitory function is N-methyl-D-aspartate receptor (NMDAR) hypofunction in inhibitory neurons
https://www.nature.com/articles/s41467-018-06512-7
It's kinda like you're turning up the flow (glutamate) to fire hose (GABA neurons) to put out a fire (inflammation or excess excitatory activity).
Goodness.
You can also see glutamate imbalances in different brain areas which different results.
This is part of why schizophrenia (and its shared illness, bi-polar) are so hard to treat.
Other studies on D-serine are equally fascinating such as this test on schizophrenia:
Significant improvement in symptoms and neuropsychological measures was noted across doses.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3111070/
What does D-serine do?
D-serine is an allosteric modulator of the brain N-methyl-D-aspartate (NMDA) receptor and potential novel treatment of schizophrenia.
It manages...glutamate activity!
You see other players as well such as magnesium (our brain's gate to glutamate).
In fact, the standard medications for schizophrenia have a fascinating effect on magnesium levels actually in the neurons themselves:
Therapy with haloperidol (a typical antipsychotic) or with risperidone (an atypical antipsychotic) both significantly raised the intracellular magnesium concentration without causing significant changes in plasma magnesium concentration.
https://www.ncbi.nlm.nih.gov/books/NBK507255/
The studies on CBD and NAC are very interesting with the latter focusing on glutamate imbalance specifically.
Let's look at a disease with close ties to schizophrenia.
Glutamate and Bipolar
Researchers found that glutamate levels were askew in young people with bipolar:
Advances in Pediatric Bipolar Research” showed that decreased concentration of glutamatergic metabolites was consistently associated with children who had a diagnosis of bipolar disorder
https://psychnews.psychiatryonline.org/doi/full/10.1176/appi.pn.2014.7a17
Interestingly depression also showed a depressed level in children while ADHD and autism showed an elevated level.
Glutamate is key to modeling the developing brain.
Separate studies delved directly into the brain to look for tell-tale signs with bi-polar:
Postmortem studies of patients with BD revealed reduced expression of NMDAR subunit NR1 in the prefrontal cortex (44) and reduced expression of several NMDA, AMPA, and kainite receptor subunits in the medial temporal cortex
https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00767/full
Again, pointing to reduced glutamate at the NMDA receptor.
The fact that it's in the prefrontal cortex would mirror depression and may speak to the depressive side of bipolar.
Adding to the confusion, a large study found that actual glutamate levels were elevated in adults:
A meta-analysis of 1H-MRS studies from 1980 to 2010 on brain glutamate and glutamine in BD showed that patients with BD had widespread increased Glx, including in the prefrontal cortex.
https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00767/full
So...low NMDA receptor activity and elevated glutamate.
This follows our tolerance instinct from above.
The brain responds to elevated glutamate levels by reducing the sensitivity and/or numbers of NMDA receptors.
It's trying to get homeostasis or balance on potentially the most toxic and important neurotransmitters in the brain.
Interestingly, scans have shown changes in brain areas tied to mood control with bi-polar and lithium.
They study glucose use (our primary energy) to pinpoint these changes and 80% of glucose consumption in the brain is from...take a guess.
Glutamate.
What about the mania side?
A study looked at patients in a manic episode in terms of glutamate levels:
Manic patients had significantly elevated Glx levels (t-test; t=–3.1, P=0.008) within the left DLPFC.
https://link.springer.com/article/10.1007/s00213-003-1440-z
Again, glutamate is the gas pedal so it's not that surprising that it might be behind mania.
Just look at Lithium.
In this slide, we see lithium inducing downregulation of NMDA receptors.
So...slowing down of glutamate activity. The issue is of course that it does this throughout the brain (think of a heavy, wet blanket).
The key is balance across various brain regions. We'll look at NAC and CBD for this balancing question.
We dive deeper into the mechanism of Bipolar in our CBD and bipolar review.
Next up...firehose fully opened.
Glutamate and OCD
OCD has recently been described as a disease of missing GABA.
Check out CBD and OCD to learn more.
GABA is the braking or calming neurotransmitter and when it's gone, the brain has an excess of potential action.
It will be applied regardless of whether there's a need and/or resolution.
You see the extreme of this with hallucinations (literally manufacturing sensory inputs) with schizophrenia.
The genetic research points the way.
There are transporters of glutamate who's job is to shuttle it away when levels are too high.
This part of the whole recycling process we discussed with astrocytes and glutamine above.
There are two major ones EEAT and VGLUT.
Look at the effects of a genetic variant of SLC1a1 which leads to EEAT activity:
2 variants, rs301434 (χ2 = 12.04; P = .006) and rs301435 (χ2 = 9.24; P = .03), located within a single haplotype block were found to be associated with transmission of OCD. Furthermore, a specific 2-marker haplotype within this block was significantly associated with OCD (χ2 = 12.60; P = .005)
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209779
This was especially true for males.
12 times the risk!
To recap...reduced ability to move glutamate out of production (the safety mechanism against excess glutamate) has a direct increase risk of OCD...by 12 times!
As we mentioned above, the balance between glutamate and GABA is key. You can't really look at OCD in terms of GABA without looking at glutamate.
GABA comes from glutamate. GABA opposes glutamate.
Speaking of repetitive thoughts and actions.
Glutamate and addiction
We already looked at the fascinating tie between THC and glutamate.
One note...addiction typically comes from repetitive use.
The theory goes that if you drink enough, for long enough, you'll eventually become an alcoholic.
- It's a process of learning (see CBD and addiction).
- The question is whether the initial repetitive use (before dopamine gets its hooks into us) is to self-medicate for imbalanced pathways.
The link between mental illness and addiction is strong and well-studied.
Each drug hits certain pathways and there are clues there:
- Nicotine and stimulants - acetylcholine and glutamate (so maybe reduced glutamate, to begin with)
- Benzos - GABA (so maybe too much glutamate)
- Alcohol - GABA and serotonin (plus just about everything) a depressant so too much glutamate?
- THC - anandamide which calms glutamate activity
Glutamate is front and center in all of these.
More importantly, addiction is a form of brain learning, and glutamate is the key to both learning and un-learning addiction.
The research on NAC is the most powerful on this front and you should check out our NAC and addiction review.
CBD is equally interesting there.
Here's the key point with glutamate and addiction…
The key to stopping the addiction may be re-balancing glutamate levels!
Accumulating evidence indicates that disruptions in glutamate homeostasis are associated with addictive disorders
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2932669/
Firepower is going to addiction circuits fed by dopamine (our reward agent) and the effects of withdrawal and tolerance.
The firepower or resource of the brain for activity is glutamate!
Here's the most fascinating piece:
Changes in the balance between synaptic and extrasynaptic glutamate levels in turn influence signaling through pre- and postsynaptic glutamate receptors, and thus affect synaptic plasticity and circuit-level activity.
Let's decipher this because it's too important.
Long term drug use impairs the ability of the brain to change!
Change at the synaptic level is required to unwind the now hard-coded addiction circuit in the brain.
The conditionally learned steps (cues - seeking - use - reward) have now had physical pathways hardwired into the brain.
The only way to unwrite those is through neurogenesis and it requires glutamate to be balanced!
Let's now move on to ways to address this pathway. One note...we're skipping over lots of other issues (autism, neuroticism, PTSD, panic disorders, eating disorders, etc).
They're all involved but we'll never get out of here and on to known ways to help balance.
Are there ways to balance glutamate activity
Some key points before we jump into CBD and NAC.
We have existing systems (multiple) to keep glutamate range-bound.
Here are the key pieces we'll focus on:
- Astrocytes and immune response
- Glutamate transporters (EEAT and VGLUTs)
- Magnesium
- GABA conversion
- Stress response
Let's start with the key player...astrocytes
Astrocytes and immune response
As we mentioned, this newly discovered rockstar is key to glutamate recycling.
There's a constant bartering system going on between astrocytes and neurons.
1 part glutamate for 1 part glutamine. Ad nauseum.
Trillions of times per second across the brain.
If astrocytes are impaired, this breaks down.
Astrocytes suffer from chronic stress, inflammation, and hyperactive immune response.
Not to mention excess glutamate (a nasty catch 22).
The key then is to support astrocyte health by bolstering the stress response system.
That just happens to be the endocannabinoid system and anandamide!
Collectively, these data suggest that AEA signaling can temper aspects of the stress response and that FAAH inhibition may aid the treatment for stress-related psychiatric disorders, such as PTSD.
https://www.ncbi.nlm.nih.gov/pubmed/30120421
The "stress" could be from infection, chronic stress, trauma, and other insults we discussed above.
Anything that pushes the system too much one way (even loss of oxygen or hunger).
No wonder people are seeking THC (which substitutes for anandamide but at too strong a level).
See CBD versus THC get a better picture.
Next up...the transporters.
Glutamate transporters (EEAT and VGLUTs)
This system needs to work well to keep glutamate under wraps.
We'll look at how NAC and CBD affect these.
EEAT is the big one and guess where it resides primarily:
Knockout of EAAT2 in astrocytes resulted in an almost complete loss of EAAT2 protein expression, but a nonsignificant reduction of glutamate uptake into synaptosomes.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5608761/
Again, this points to controlling inflammation which is toxic to astrocytes.
Astrocytes also maintain the blood-brain barrier which is the main defense against brain inflammation.
Brand new research on Lipoic acid (an amino acid) and Vitamin D are interesting:
In our study, the combination of LA and vitD showed beneficial effects on the viability of astrocytes, since the substances are able to cross the brain barrier.
https://www.hindawi.com/journals/omcl/2019/2843121/
That was a study on neurodegeneration and aging with a focus on inflammation.
You can supplement ALA (alpha-lipoic acid) and Vitamin D3.
Next up...the gatekeeper.
Magnesium
People swear by magnesium for sleep, calm, and migraines.
What's the key?
Magnesium just happens to be a block that fits in the glutamate receptor.
In fact, it has to be removed in order for activity to continue!
It's an integral player in the checks and balance of glutamate levels in the brain.
For that reason, consider any of the "ates" like magnesium glycinate, theorate, citrate, etc.
Big review of magnesium glycinate for sleep, anxiety, stress response, and more.
Glycinate has been a game-changer for me personally with migraines. They're gone after 40 years. Another example of glutamate/GABA mismatch!
Then there's the other side of the coin.
GABA conversion
How can we support something so basic as the balance between GABA and glutamate (besides NAC and CBD below)?
The enzyme and gene in charge of this is GAD.
There's intriguing new research from the keto world on this process.
According to this formulation, in ketotic brain astrocyte metabolism is more active, resulting in the enhanced conversion of glutamate to glutamine. This allows for: (a) more efficient removal of glutamate, the most important excitatory neurotransmitter; and (b) more efficient conversion of glutamine to GABA, the major inhibitory neurotransmitter.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2722878/
Goodness. That's the holy grail of this whole article, right?
Again, it points to the astrocytes again.
Finally...the key to all of this.
Stress response
We're using stress in the general meaning...anything that pushes on the system.
Stress spikes glutamate, suppresses astrocyte activity, and eats up GABA.
This is a great place to really get to know the endocannabinoid system.
It is THE stress response system in the body!
Let's let the researchers phrase it:
The endocannabinoid (eCB) system has emerged as a central integrator linking the perception of external and internal stimuli to distinct neurophysiological and behavioral outcomes (such as fear reaction, anxiety, and stress-coping), thus allowing an organism to adapt to its changing environment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5871913/
Read that back over just one more time.
It turns out that astrocytes were thought to be bystanders in the brain with just a supporting role to neurons.
No no no!!
New research is showing they're as influential and their means of action is through the endocannabinoid system:
Therefore, astrocytes respond to endocannabinoids that then potentiate the synaptic transmission, indicating that astrocytes are actively involved in brain physiology.
https://www.sciencedirect.com/science/article/pii/S0896627310006860
Endocannabinoids are the fuel for astrocytes to action!
We would then expect to see effects from CBD on astrocytes and glutamate.
What a segue.
CBD and glutamate balancing
We've covered the other side of the coin in our CBD and GABA review.
We'll break it up into three areas:
- Research on CBD and the glutamate pathways above (astrocytes, stress response, GABA conversion)
- Research on CBD and glutamate directly
- Research on mental health issues directly tied to glutamate
Lots to cover...let's get started.
Before we get started, let's look at the beauty of CBD.
Most chemicals push a pathway in one direction or another.
SSRI's are an example of this for serotonin and Benzos for GABA.
The downside to this is that the body pushes back and that creates a spiral of tolerance and suppressed function.
Check out CBD and tolerance or CBD and withdrawal to understand this.
Even the other cannabinoids like THC operate this way which is why THC long term can set up the brain for depression and anxiety (see problems with high THC).
CBD works very differently which is why we don't see tolerance, overdose, or withdrawals.
Technically, it's all an allosteric modulator.
That's a mouthful...let's break it down because it's why CBD is so fascinating.
Let's say a signal goes from neuron A to B.
CBD boosts the signal backward from B to A as feedback!
- Too much of substance A, back off.
- Not enough of substance A, send more!
This sounds incredulous but we see it all over pathways that are completely not connected.
The effects on cancer are easiest to understand:
- Healthy cell with low inflammation - CBD has no effect
- Healthy cell with high inflammation - CBD decreases inflammation
- Cancerous of infected cell - CBD INCREASES inflammation
Read that back over because it's critical to CBD in the body. There are three different effects depending on the state of the system.
Why would CBD increase inflammation in faulty cells?
This is the natural check the body uses on bad cells. Oxidative stress is the weapon to kill off wayward cells.
Essentially, chemo and radiation create massive spikes in oxidative stress!
So...we now know that CBD works within the endocannabinoid system (tasked with balancing other key systems) as a feedback mechanism.
Let's jump into glutamate.
Research on CBD and the glutamate pathways above (astrocytes, stress response, glutamate transporters, GABA conversion)
First astrocytes, a pivotal (half really) piece of the glutamate balancing system.
This is the new superstar in neuroscience.
What about CBD there?
CBD's impact on astrocytes (as well as neurons and microglia) are strongest in terms of neuroprotective effects.
Decreasing the inflammatory responses of either microglia or astrocytes were shown to be a critical component of the neuroprotective process [31]. CBD is a potent regulator of oxidative stress, a leading cause of neurodegeneration, as it scavenges the reactive oxygen species (ROS) and reduces lipid peroxidation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5578059/
Another study looked at CBD's effect on astrocytes after hypoxia (loss of oxygen).
CBD also reduced neuronal death and microglial activation and improved neurobehavioral losses following the insult. Interestingly, the effect on astrocyte activation was observed only at day 15 post HI, and not earlier at day 7
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5578059/
Another study looked at the effects of CBD on common inflammatory markers with Alzheimer's:
In addition, it was shown that CBD decreased GFAP and S100β levels, NF-κB pathway activation, and iNOS and IL-1β levels in Aβ-stimulated cultured newborn rat astrocytes
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5578059/
That's a litany of inflammatory agents that can wreak havoc on a brain.
There are lots of studies.
Let's look at stress response since this is key to the damage done to astrocytes.
We'll reintroduce anandamide, our system's natural stress buffer.
What does CBD do there?:
Biochemical studies indicate that cannabidiol may enhance endogenous anandamide signaling indirectly, by inhibiting the intracellular degradation of anandamide catalyzed by the enzyme fatty acid amide hydrolase (FAAH)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3316151/
We covered FAAH in-depth since people lacking it can't feel pain, anxiety, or depression.
Basically, FAAH eats up anandamide and CBD blocks FAAH.
This speaks to CBD's ultimate effect:
It was also found that CBD has a clear anti-stress effect after either acute or repeated administration, attenuating the behavioral and autonomic consequences of acute restraint stress (31, 32) and the anxiogenic effects of chronic unpredictable stress
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6161644/
What about the glutamate/GABA balancing act?
Let's look at a fascinating study on CBD's effect on GABA/glutamate with autism.
They found the following (we'll decipher):
Across regions, CBD increased GABA+ in controls, but decreased GABA+ in ASD; the group difference in change in GABA + in the DMPFC was significant. Thus, CBD modulates glutamate-GABA systems, but prefrontal-GABA systems respond differently to ASD.
https://www.ncbi.nlm.nih.gov/pubmed/30758329
Translation, please.
Essentially, CBD would increase GABA but reduce it in people with autism. This effect was most prominent in the prefrontal cortex for people with autism.
Why is this interesting?
Newer studies point to the hyporfunction of glutamate in this area and a resulting protective measure of the brain to suppress glutamate function.
We found a significant decrease in the cingulate N-acetyl-aspartate (NAA) and the combined Glu and glutamine (Glx) signals in adults with ASD,
https://www.nature.com/articles/mp201462
So, CBD did not boost GABA in a specific brain area where glutamate was low.
Remember that GABA offsets or constrains glutamate.
This was the opposite effect of what happened in people without autism.
Two different results depending on the state of the system
We have done a full review of CBD and autism.
That's a great lead into CBD and glutamate balancing directly.
Research on CBD and glutamate directly
Let's look at some of the interesting studies on CBD and this pathway beyond the autism study above.
First, a study looked at how CBD would affect the NMDA receptors following opioid abuse.
Glutamate activity and sensitivity have been implicated in both neuropathic pain and opioid system dysregulation.
CBD was shown to normalize the imbalanced NDMA activity:
Thus, CBD displays antagonist-like activity toward σ1R to reduce the negative effects of NMDAR overactivity in the abovementioned experimental situations.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142691/
The key there is "NMDAR overactivity".
This is key to offsetting the imbalance in the glutamate system.
Remember how we said too much glutamate can be toxic to the brain?
CBD's effect:
CBD exhibits antioxidant properties and protects neurons from glutamate-induced death but without cannabinoid receptor activation or NMDAR antagonism
Another fascinating study looked at CBD's effect on glutamate/GABA conversion following early exposure to infection (key to schizophrenia).
It's known that early exposure to certain viral infections can cause glutamate imbalance later on.
Remember, the immune system (astrocytes, etc) is heavily involved in glutamate management and it can be primed to overreact.
Their findings:
CBD treatment attenuated poly I:C-induced deficits in cannabinoid CB1 receptor binding in the PFC and glutamate decarboxylase 67, the enzyme that converts glutamate to GABA, in the HPC.
https://www.ncbi.nlm.nih.gov/pubmed/31202911
Let's translate that because it's too fascinating.
Basically, early infection would lead to later poor function in the CB1 receptor (main endocannabinoid receptor) and another key piece…
glutamate decarboxylase 67
That's the enzyme that flips the switch from glutamate to GABA! Remember that GABA is made for glutamate (go figure).
After early infection, the switching mechanism would run low later in life.
CBD offset this drop!
People...this is the key to glutamate (gas pedal) and GABA (brake pedal) balancing!
It's also why there ties to almost every mental health issue we listed above and early (and later) trauma, infection, and stress.
We did a big review on trauma and CBD.
We talked quite a bit about ketamine above in the depression area which directly interacts with NMDA receptors and glutamate.
An interesting study looked at CBD and ketamine in conjunction:
CBD significantly augmented the activating effects of ketamine, as measured by the activation subscales of the BPRS. However, CBD also showed a non-significant trend to reduce ketamine-induced depersonalization, as measured by the CADSS.
https://www.ncbi.nlm.nih.gov/pubmed/21062637
So...it boosted the positive effects (BPRS measures effects on anxiety, depression, and other issues) while offsetting the negatives of ketamine (CADSS).
This would imply a similar effect in the glutamate system and we're not surprised by the offset considering research on CBD and schizophrenia (two different effects on dopamine depending on brain area).
A study on Alzheimer's looked at CBD multiple pathways in addressing brain protection:
CBD has several features that may be exploited for the treatment of AD, including the prevention of glutamate-induced excitotoxicity, reduction of proinflammatory mediators, and the ability to scavenge reactive oxygen species (ROS) and reduce lipid peroxidation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938896/
This is a laundry list of defensive measures for our brains. glutamate excitoxicity!
Redlining the brain's engine...everything we've been discussing.
Finally, a great study that shows how glutamate is interwoven into every other pathway (serotonin, dopamine, opioid, etc).
A group of researchers looked at CBD's effect following the fall-out of injury in mice.
This usually results in an imbalance in serotonin and glutamate.
CBD's effect:
In vivo microdialysis revealed that the administration of CBD significantly enhanced serotonin and glutamate levels in vmPFCx in a different manner depending on the emotional state and the duration of the treatment.
https://www.ncbi.nlm.nih.gov/pubmed/26711860
Let's break that down because it's too cool.
First, above, we showed how CBD could reduce glutamate if too high.
Here, it's enhancing it if too low in a specific area...the prefrontal cortex!
The fascinating piece is "depending on emotional state".
Again, we don't want to just pump up serotonin (like SSRIs do) or glutamate in one direction.
Okay...those are all interesting but are there effects on diseases directly tied to glutamate imbalance?
Yes!
Research on mental health issues directly tied to glutamate
We'll quickly look at these mental health issues that are intimately tied to glutamate:
- Seizures
- Anxiety
- Depression
- Schizophrenia
Very different mental health issues strongly linked with glutamate...what's CBD's effect in research?
Seizures
This was CBD's original claim to fame.
The effect of the endocannabinoid system including anandamide:
In the CNS, CB1 receptors are expressed pre-synaptically on both glutamatergic and GABAergic interneurons, and activation of these receptors results in inhibition of synaptic transmission, including glutamate release
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5767492/
It slows down the activity which leads to seizures.
Another study looked at cocaine-related seizures:
In conclusion, CBD protects against seizures in a model of cocaine intoxication. These effects possibly occur through activation of mTOR with a subsequent reduction in glutamate release.
https://www.ncbi.nlm.nih.gov/pubmed/26283212
Next up, an issue close to heart (our amygdala...technically).
Anxiety
Glutamate is all over anxiety even if it's disguised as GABA, it's yin/yang twin.
We've covered the pathways extensively and you can reference all the aspects at our CBD and anxiety research article.
A well-designed study (double-blind, placebo) looked at CBD's effect on anxiety with the following results:
Anxiety scores decreased within the first month in 57 patients (79.2%) and remained decreased during the study duration.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6326553/
Our favorite reviews:
Lots of research across dozens of reviews.
Next up, anxiety's an all too familiar cohort.
Depression
We looked at CBD and depression here in detail (maybe too much detail).
First, glutamate and serotonin are intimately tied together.
In fact, serotonin manages glutamate pathways differentially across the brain:
In the CNS, 5-HT exerts a very complex modulatory control over glutamate- and GABA-mediated transmission, involving many subtypes of 5-HT receptors and a large variety of effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430669/
That article shows a kaleidoscope of nuanced interactions between the two.
If glutamate is the gas pedal of our brain, serotonin is the driving wheel.
Afterall, serotonin manages ALL human behavior.
It's intimately tied to depression through its effect on neurogenesis via the brain's fertilizer BDNF.
Check out CBD and neurogenesis or CBD and BDNF for full detail but a quick look:
CBD appears to stimulate synaptic plasticity and facilitates neurogenesis that may explain its positive effects on attenuating psychotic, anxiety, and depressive behaviors.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938896/
And to show we're not making this stuff up:
The mechanisms underlying these effects involve multiple cellular targets to elevate brain-derived neurotropic factor (BDNF) levels, reduce microglia activation, and decrease levels of proinflammatory mediators
So...we have both the growth side (BDNF and neurogenesis) and protection from the insulting side (microglia hyperactivation and inflammation).
The microglia is the immune system...see CBD and microglia here.
Their cohort? Astrocytes!
What about one of the most complicated and frustrating diseases around.
CBD and Schizophrenia
We have a comprehensive look at CBD and schizophrenia:
CBD significantly reduces psychotic symptoms in acute schizophrenia with a potency similar to that of the antipsychotic amisulpride
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342457/
It rivaled a key drug used (which is not terribly successful) without the nasty side effects.
Remember how CBD would counter the schizophrenia-like effects (depersonalization, etc) of ketamine.
We know that ketamine's primary effect (you can never say solely in the brain) is via the glutamate pathway.
We also saw how CBD would normalize both serotonin and glutamate activity in mouse models of schizophrenia following early-life infection.
Check out the full review of CBD schizophrenia. It's probably the most exciting result for CBD (aside from addiction).
Hopefully, we showed how CBD might be an interesting modulator of glutamate pathways that lies at the heart of almost every mental health issue (plus pain, addiction, neurodegenerative diseases).
Next up, the research that really opened our eyes.
NAC and glutamate for mental health
We admit it. We were GABA centric and glutamate agnostic.
This derives from both the current means of treating anxiety, insomnia, etc (benzos) as well as the established mechanisms for anxiety which we studied for months.
You can't look at GABA without glutamate. It derives from glutamate after all!
NAC broke that wide open.
We're almost as impressed with NAC as with CBD!
NAC's primary role is to support glutathione, our body's main antioxidant.
See CBD and glutathione.
Glutathione has a side job we mentioned above. It acts as storage or sink for glutamate along with its partner's cysteine (come from NAC) and glycine.
Glutamate and glycine are readily available in the brain...cysteine is the main rate-limiting factor for glutathione.
We don't go into full detail here for NAC since we've written extensively at our NAC and mental health review but the research is very compelling.
CBD and NAC could be powerful allies for almost every mental health issue we've come across including very disparate ones.
NAC supports glutamate balancing and our detox (redox) pathways while CBD supports the endocannabinoid system which governs the nervous system, endocrine system (hormones), and immune system.
Goodness. If you've read this far, hopefully, the payoff was worth it.
Let's get practical.
How much CBD and NAC for glutamate balancing
We actually have some good research on this front.
First CBD.
The maximum daily dose for neurogenesis (key to rebuild/repair pathways) is 300 mg per day.
After that, it starts to go down even if other attributes continue (anti-anxiety, anti-psychotic, etc).
It's been tested at 600-800mg for more serious issues but long term, 300mg appears to be best for neurogenesis (the Holy Grail!).
As for NAC, most of the studies were around 1800-2000 mg per day.
Most brands come in at 600 mg per capsule or 1000 mg. We use this one.
Safety for both CBD and NAC at the 300 mg and 2000 mg respectively is very strong.
Always work with your doctor or naturopath with any new supplements as they can interact with other medications.
What about the type of CBD and NAC?
The best CBD and NAC for glutamate balancing
First, for CBD, there are baseline requirements:
- Organically grown in the US at FDA registered farms
- CO2 processed
- 3rd party tested (we test ours twice)
- No THC (THC works in one direction as an agonist of CB1 activity)
- No pesticides
- No heavy metals
- No solvents
- No mold
- No bacteria
This is a baseline and our results are at the top of each page.
Then there's the question of CBD full spectrum versus isolate.
We've looked at 100's of NIH studies on CBD across our website.
Guess what...they're all based on CBD isolate. That's one reason we focus on isolate.
The bigger one is simple.
40-60% of the population has allergy/histamine issues.
Full-spectrum CBD is likely to cause reactions here.
In fact, our first exposure with 3-4 of the biggest brands (full spectrum) did not go well (allergic reactions).
We tried CBD isolate and all that went away. That's when we decided to start IndigoNaturals.
Here's the bigger issue in terms of allergic responses:
Histamine elicits glutamate release from cultured astrocytes.
https://www.ncbi.nlm.nih.gov/pubmed/29858014
That's' going the wrong direction based on everything we've discussed!
As for NAC, we like the Now brand at 600 mg or 1000 mg.
We have no doubt that you'll see plenty of headlines (maybe watered down) in the next few years for glutamate and CBD/NAC specifically.
Be well. Take care of each other!
Related Research:
Gaba Guide
Immune system as the future of mental health
THC and glutamate
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.