CBD and Psilocybin - Psychological Trauma Pathways
It surrounds us.
In particular, recent epidemiological studies have demonstrated high rates (70%-80%) of lifetime traumatic experiences, suggesting that previous epidemiological surveys may have underestimated the prevalence of traumatic event
That number's probably low. Everyone is touched in some way by trauma. Or infection (we'll see why they're the same to the brain below).
When you dig deeper into everyone's past (and their ancestor's past), there are events that continue to push and pull on current mental status and how people interact with the world, each other, and themselves.
Trauma is everywhere and it carries a chemical and structural memory in the brain.
Like water finding the lowest path, current brain function will flow through these channels as they've literally been carved into the architecture of the brain.
We'll go deep into this process but more importantly, we'll look at how to "unwind" or unlearn this past's trespass.
Trauma intersects with addiction, mental illness, and even our immune system as we'll see below.
We can then turn CBD and psilocybin into powerful tools to overwrite the effects of trauma.
There's a very powerful pathway lurking right behind serotonin that holds the key.
- Why can some people experience warfare and not get PTSD while others are haunted by it?
- How do early traumas such as difficult childbirths or infections in the 3rd trimester linger on?
- Can trauma in prior generations show its card in us as we live and breath now?
Once you unravel the onion, you'll see that this may be the most important piece to deal with first for mental health and addiction which are results and coping mechanisms for the original insult.
Here are the topics we'll cover:
- A lay of the traumatic landscape
- Trauma and the brain
- Trauma and the Default Mode
- Trauma and neurotransmitters or stress hormones
- Trauma and immune system
- Hormone and gender effects on trauma
- Stress response and trauma (hello Anandamide)
- BDNF and neurogenesis for trauma
- Research on CBD and trauma
- Research on psilocybin and trauma
- How much CBD or psilocybin for trauma
- What's the best CBD or psilocybin for trauma
It's a lot but we'll focus on aspects we can actually positively affect to unwind trauma.
Let's get started.
A lay of the traumatic landscape
We covered a great deal of the hard research in our CBD and PTSD review but let's zoom out a bit for the broader area of trauma itself.
We'll look at these facets surrounding trauma:
- Age at which it occurs
- Intensity and frequency of the event
- Gender differences with trauma
- Individual differences tied to trauma response
These aspects actually shed light on what's going so let's start with a 40,000-foot view.
We all know that trauma is any intense or prolonged negative event that people encounter.
It can run the gamut from accidents, rape, abuse, and more, unfortunately.
Even social isolation or rejection elicits a form of trauma as the brain only has one way to deal with such events.
Trauma can occur even before we have memories such as with difficult births and even past generations.
there was evidence suggesting that Holocaust survivor offspring show a heightened vulnerability for stress, although this was only evident in the face of actual danger.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6720013/
But our genes aren't changing so what drive's this "memory"?
There's a layer of coding above our genes called epigenetics that decides what genes to turn on and off.
This is where traits from ancestors can get passed down including how we process stress.
We'll cover that separately below.
A great deal of the impact from a traumatic event depends on the age at which it happened.
Trauma experienced before age 13 had a higher risk for PTSD later in life:
In the childhood group conditional risks for PTSD and major depressive disorder were 17.0% and 23.3%, respectively, compared with risks of 13.3% and 6.5%, respectively, in the adolescent group.
https://www.ncbi.nlm.nih.gov/pubmed/15172941/
This makes sense since the brain is undergoing massive developmental changes.
The traumatic event is literally being woven into the framework of the developed brain.
Like drawing your name in wet concrete.
In the end, a brain is a prediction machine. It hates the unknown and tries to anticipate the future based on the past.
If there was a dangerous situation that occurred during formation, it will ramp up systems needed to be more vigilant as it assumes the body exists in a more dangerous world.
- Vigilance
- Aggression
- Fear
All pretty sensible responses to keeping you alive after trauma is "baked" into brain formation.
We'll see the actual pathways of how this happens below.
This is a form of learning really. Yes, it is maladaptive, but just like addiction, it rests on learning.
The key point is this...learning in the brain is a physical thing.
Literally baked into the architecture. That's why is so difficult and long-lived (like addiction).
In fact, very early trauma back to the second and third trimester in the womb can show up later in life across the mental health spectrum.
Prenatal stress has also been shown to increase the stress reactivity of infants,51 which is of particular importance given other studies showing that early stress reactivity is connected to emotional temperament later in life
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5052760/
Literally, early exposure to stress (or infection) is "priming" the baby's system to respond more strongly to stress when they get older.
The stress response is literally the pathway for trauma response as we'll see below.
The mechanism for this change is via architecture in the brain, the epigenome (the control panel for our genes), and of all things...the immune system!
The good news is that these are both malleable with the first being more difficult.
Let's jump to the brain first since this "hardwired" piece is what makes trauma so sticky.
Trauma and the brain
We're going to focus down on three key brain areas:
- Hippocampus - the seat of memory and mood control
- Amygdala - the fear or anxiety (as well as other emotions) circuit
- Prefrontal cortex - our rational overseer
Don't take our word for it:
Brain areas implicated in the stress response include the amygdala, hippocampus, and prefrontal cortex.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/
The hippocampus is really critical to trauma.
Not only does it manage the actual memory of the traumatic event but it governs the interaction with our emotional coloring of it via the amygdala.
More importantly, there are known correlations with trauma and the hippocampus:
Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2819093/
Before we go pinning our traumatic response on a pre-given brain area size, it's important to understand the hippocampus' unique place in the brain.
It's the area of greatest change!
It has to be...since memories are made every second of your life.
That plasticity (a fancy word to say it can change) is also its greatest weakness.
It's very susceptible to the various insults of the brain:
- Infection and inflammation (see CBD and neuroinflammation)
- Chronic stress
- Hyperactive immune response
- Oxidative stress (see CBD and oxidative stress)
- TBI (see CBD and TBI)
- Trauma
In fact, the hippocampus' resilience may be part of the difference in how we experience trauma.
Gurvits et al147 showed bilateral hippocampal volume reductions in combat-related PTSD compared with combat veterans without PTSD and normal controls.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/
Again, we have a giant review on CBD and PTSD which really drives down into the pathways.
Aging and loss of estrogen (perimenopause) or testosterone will slowly eat at hippocampus volume on their own.
Trauma, however, can be a massive hit to it.
This is critical because hippocampus function is tied to almost every mental health issue you can think of.
It's also one of the few brain areas that can grow! That's our saving grace and we'll cover it in detail below.
Then there's the amygdala, our emotional control unit.
Basically, the amygdala "colors" experience with an emotional quotient, and the more intense this shading, the more powerful the memory.
Sound familiar?
If the amygdala is too active or strong, it's intimately tied to anxiety (see CBD and pathways of anxiety).
On the other side is the prefrontal cortex which is our rational push back against the more emotional amygdala's signal.
This supports the idea that the vmPFC has a general role in the suppression of amygdala activity
In fact, this area gets temporarily shut down during puberty for remodeling and we don't have to describe the rational to emotional mismatch there!
Both undergo changes from trauma.
The amygdala can get bigger (stronger) from the trauma that occurs in childhood. It can get smaller if experienced during adulthood.
The prefrontal cortex can actually shrink which is the tie between early trauma and depression (see CBD and depression).
So...now we have a too strong fear response with less rational push back.
Anxiety. Panic.
The connection between these two is also changed!
This suggests that traumatic life events disrupt the normal pattern of mPFC and amygdala regulation
Essentially, the communication between these two areas is disrupted by trauma.
This leaves the amygdala (fear and emotional response) to run without check.
That link walks through so much research on this whole topic...excellent source!
Our main takeaway is that trauma alters the brain's connectivity and volume in key areas.
The key to correcting that is neurogenesis which we'll use an entire section below to focus on.
Trauma and the Default Mode
One quick detour and it's really important.
Our brain activity can be in different states and there are two big ones to look at with trauma.
- Default Mode
- Active mode
The default mode is a passive state...think of daydreaming, mind wandering, etc.
You're not actively concentrating on a task at hand but drifting into the future or internal affairs.
Why is this important with trauma?
There's a peculiar effect with trauma that becomes very pronounce with PTSD where you feel like you're reliving the original experience.
It can be called flashbacks but the fear and emotional state can be re-created almost exactly.
You're feeling it all over again.
The default mode is key to this.
It's also your historical autobiography...everything good or bad that makes you!
Decreased within-DMN connectivity and disrupted DMN-SN and DMN-CEN coupling could form the basis for intrusive trauma recollection and impaired episodic autobiographical recall in PTSD.
https://pubmed.ncbi.nlm.nih.gov/30831461/
Let's translate the Klingon please.
Essentially, there was less connectivity between the amygdala and prefrontal cortex (we covered above) but more in the default mode.
It's as if the trauma has broken through to our daydreams. In that respect, it sits outside our focus and lurks like a specter.
Excuse our colorful language but this is all very recent research that newer gen brain scans had to find.
The combination of our default mode activation and the heightened fear response and memory combine for a fear that's "locked-in".
This is really important when we get to psilocybin so just make a mental note.
Let's turn to the messengers of the brains...neurotransmitters.
Trauma and neurotransmitters or stress hormones
We're going to focus on trauma and the following powerful messengers:
- Serotonin - manager of all human behavior and key stress responder
- GABA/Glutamate - the brake and gas pedal of the brain
- Cortisol - a primary stress hormone
- CRF - initiates the stress response cascade
That's a lot to chew off but it's really important.
Let's start with serotonin.
Serotonin and Trauma
We've covered serotonin in-depth at our CBD and serotonin review.
It's the master regulator of all human behavior but we'll focus on its stress response function and the less known but all-powerful pathway called BDNF.
Serotonin is usually called the "feel good" chemical but that belittles its role and scope of responsibility. It's a master regulator in the brain...or orchestrator if you will.
It's more like the "feel right in your body" chemical.
Trauma has a direct effect on serotonin function even if it occurs years or decades before.
Serotonin is our first line of defense against stress and trauma.
In fact, reduced function in serotonin can affect how we respond to trauma even if early in life:
Childhood trauma interacts with low expressing 5-HTTLPR genotypes to increase the risk of suicidal behavior among patients with substance dependence.
https://www.nature.com/articles/1301331
5HT is short for serotonin. If a person has a version of the gene that generates low serotonin function, early trauma was more likely to lead to depression, addiction (just a reflection of this reduced serotonin), and suicide LATER in lfe.
This is especially true for early life (before age of 5) but in general, serotonin directs our stress response:
Coping is the major determinant of stress resilience. Brain serotonin transmission is critical for coping strategies. Serotonin driven prefrontal cortical–amygdala determines active or passive coping outcome
https://www.sciencedirect.com/science/article/abs/pii/S0166432814005087
We have a giant review on supporting resilience.
We'll look at how to address serotonin depletion with CBD (and other tools) below.
One note… serotonin is the target for SSRIs (antidepressants) like Effexor, Prozac, Lexapro, and others.
The issue is that these build tolerance with use which we covered in our CBD versus SSRIs here.
That's a major class of medications that tells you just how important serotonin function is with trauma.
Wait till you see how they really work in the BDNF section below.
Let's turn to the gas and brake pedals of the brain.
Trauma and GABA/Glutamate
Anxiety, panic, OCD, PTSD, and the whole (hyperexcitable) spectrum of issues is intimately tied to an imbalance in GABA/Glutamate.
In fact, GABA is THE pathway for anxiety, insomnia, and seizure.
How does trauma affect GABA?
Just this…
This study found that juvenile traumatic stress-induced chronic anxiety and spatial memory loss and reduced expression of GABAAR subunits in the adult rat brains.
https://www.hindawi.com/journals/np/2017/5715816/
Trauma can downregulate GABA function going forward!
This is not good since GABA keeps glutamate (gas pedal) at bay and too much glutamate is toxic to the brain.
Especially in the hippocampus (memory/mood control) and prefrontal cortex (push back on fear).
It's this "lever down" effect of trauma that keeps causing issues going forward.
We look at CBD and GABA and CBD and glutamate since they're so important.
Alcohol and benzos drive GABA function (till tolerance sends it backwards)...see where the self-medication comes in?
So we want to support GABA so we don't continue damaging the brain pathways.
A quick detour to our stress hormone cascade.
Trauma and cortisol
Cortisol is our primary stress hormone.
This is another system that gets ratcheted up from prior trauma.
A history of childhood trauma has longstanding effects on adulthood cortisol responses to stress, particularly in that depressed individuals with a history of childhood trauma show blunted cortisol responses
https://pubmed.ncbi.nlm.nih.gov/25265282/
Essentially, the cortisol system is upregulated from trauma and as a result, stops working with time.

This is very common and we see it with GABA and pain, anandamide and inflammation, etc.
If a system is constantly hit too hard, the body will actually reduce receptor numbers and sensitivity which causes a whole different problem.
It's important to get cortisol under control as it works as a memory of the original trauma:
The stress hormone cortisol strengthens memories of scary experiences. However, it is effective not only while the memory is being formed for the first time, but also later when people look back at an experience while the memory reconsolidates.
https://www.sciencedaily.com/releases/2015/07/150701083336.htm
Between the emotional memory (amygdala and hippocampus) and the sheer "feeling" memory or cortisol, it serves to relive if not reinforce the original trauma.
This locks a specific pathway into the brain.
One more stop.
CHR and trauma
Corticotrophin releasing factor starts the whole stress response process. It initiates and cortisol follows orders.
Early life stress can skew this process which raises the risk of poor response to trauma when it occurs:
Corticotropin-releasing hormone (CRH) is disrupted in individuals with PTSD and early-life stress and hence may mediate the effects of early-life stress on PTSD risk
https://www.nature.com/articles/npp2015338
The net takeaway is this.
We have various systems that are used to manage stress. They can be overwhelmed by traumatic experiences and skewed going forward with powerful effects on mental health and addiction.
We'll look at anandamide and the endocannabinoid system below with CBD to discuss our powerful stress response backup!
We have to talk about the immune system.
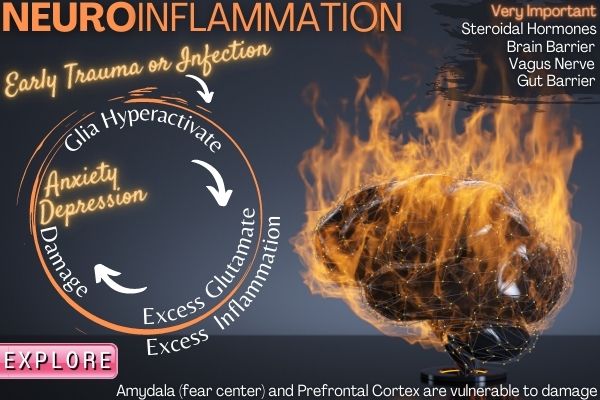
Trauma and immune system
You're probably wondering…"Why on earth are we discussing the immune system and trauma"??
The immune system responds to any threat and trauma is a threat.
It does so with its primary tool...inflammation!
The analysis demonstrates that childhood trauma contributes to a pro-inflammatory state in adulthood, with specific inflammatory profiles depending on the specific type of trauma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4564950/
Okay...so what?
Systemwide inflammation invariably means brain inflammation.
All the new research is pointing to the powerful effects of neuroinflammation on mental health!
Check out CBD and neuroinflammation to learn more.
Remember the "gas pedal" neurotransmitter above? Glutamate?
When the immune system runs hot, it causes a rush of glutamate from immune sentries called microglia.
This causes actual damage in the brain and lies at the door of depression, anxiety, and a range of issues.
The prefrontal cortex and hippocampus are especially vulnerable to this assault.
It's not just mental health:
Comparing more than 106,000 people who had stress disorders with more than 1 million people without them, researchers found that stress was tied to a 36 percent greater risk of developing 41 autoimmune diseases, including rheumatoid arthritis, psoriasis, Crohn's disease and celiac disease.
https://medicalxpress.com/news/2018-06-severe-stress-immune-overdrive.html
We have to address this inflammatory state as well and we'll cover tools there.
Let's turn to steroidal hormones and gender.
Hormone and gender effects on trauma
Interestingly, there are some differences in trauma response between genders.
When both sexes experience the same type of trauma, females are still more likely to develop PTSD and report more chronic symptoms as compared to males
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7048196/
The steroidal hormones, testosterone, estradiol, and progesterone, have very different impacts on the role of trauma.
We'll start with the dominant female hormones estradiol and progesterone.
Estradiol directly drives serotonin, our primary stress response buffer (see estrogen and mental health).
Progesterone directly drives GABA (see Progesterone review or postpartum depression and allopregnanolone).
Goodness….progesterone drops by 50% at age 40 on average and estradiol goes into free fall around age 47 (see why perimenopause can be so hard).
These two hormones are tied into every cell and every system of your body.
Then there's testosterone.
A look at combat veterans:
pre-deployment testosterone levels predicted the development of PTSD symptoms at 1 and 2 years post-deployment.
https://pubmed.ncbi.nlm.nih.gov/25128222/
Testosterone has as a general "it's all going be fine" effect on resilience.
Studies bear this out in terms of trauma:
Given its role in social behavior and positive mood, it is not surprising that blood and saliva testosterone levels decrease following stress (Morgan et al., 2000a) and that low circulating levels are often found in individuals with PTSD or MDD
https://www.sciencedirect.com/science/article/pii/S2352289514000058
Testosterone drops about 1% each year starting around age 18-20.
One final player...DHEA.
DHEA is the mother hormone that breaks down into testosterone, estrogen, and more.
They found that soldiers with more DHEA performed better during the final underwater navigation exam than those with less DHEA. These findings are being published by Elsevier in the August 15th issue of Biological Psychiatry.
We bring this up since DHEA can be supplemented! Get all your steroidal hormones tested!
Let's look at the endocannabinoid system where CBD works.
Stress response and trauma with a focus on endocannabinoids
We've looked at key stress response buffers since that since is dysregulated by trauma long term:
- Serotonin - general stress manager which gets exhausted trauma
- GABA - immediate "brake pedal" on brain activity tied to anxiety and fear
- Steroidal hormones including estradiol, progesterone, and testosterone
Let's now turn to the system tasked with balancing all other key systems when out of balance...the endocannabinoid system.
We all have one...it dates back about 600 million years and we share it with all animals.
This system is tasked with balancing other key systems including:
- Neurotransmitters - serotonin, GABA, and more
- Immune system - inflammation and cellular birth/death cycles
- Endocrine system - hormones including both steroidal and metabolic
Let's focus down on one of our two main endocannabinoids that's in every cell of your body right now.
Anandamide. Named after the Hindu goddess of "bliss", Anand.
If serotonin is our front-line defense against stress and trauma, anandamide is the ready-call backup.
Increased anandamide (AEA) signaling through inhibition of its catabolic enzyme fatty acid amide hydrolase (FAAH) in the basolateral complex of amygdala (BLA) is thought to buffer against the effects of stress and reduces behavioral signs of anxiety and fear.
https://www.jneurosci.org/content/39/7/1275
In fact, it's made as needed and almost immediately broken back down.
THC, the psychoactive part of cannabis (see THC versus CBD) mimics anandamide but it hangs around too long and is too strong.
With longer-term use, the body will actually downregulate this pathway which is the wrong way to go.
CBD doesn't build tolerance and is not habit-forming.
It does, however, support anandamide when low (we'll see below in the CBD section).
Why does that matter?
Scientists from Leiden University in the Netherlands have shown that anandamide — a natural cannabinoid produced by the brain — could help people to forget traumatic memories and reduce stress levels.
https://www.medicalnewstoday.com/articles/bodys-own-natural-cannabinoid-may-erase-traumatic-memories
Goodness...this is the Holy Grail of trauma.
This is probably why trauma victims are so drawn to cannabis but again, there's an issue there with THC in terms of tolerance.
We don't want to actually reduce CB1 (the receptor where both THC and anandamide do their magic) long term with THC.
We'll cover other tools to support this system below.
Let's now turn to the most important piece of this entire article in terms of unraveling trauma.
BDNF and neurogenesis for trauma
If you're still with us...take a deep breath.
This is really important and we're now turning the tide from everything bad about trauma to the mechanism of how to heal from it.
BDNF is short for brain-derived neurotrophic factors. That's a longwinded way to say it's our brain's fertilizer.
We've covered every major mental health issue (see CBD and mental health) and they all circle around BDNF.
Here's the 40,000-foot view.
The brain is under constant assault from various directions:
- Stress
- Trauma (ding ding ding)
- Infection
- Inflammation
- Excessive glutamate
- Oxidative stress
All our highly destructive to actual brain material and prior trauma directly affects stress response, inflammation, glutamate, and oxidative stress.
What's holding back the dam of damage?
BDNF (and some cohorts).
BDNF is tasked with rebuilding, replenishing, and most importantly for trauma...rewriting brain pathways and architecture.
So let's look at trauma directly.
First, what about gene variations for BDNF?
Our data demonstrate that in patients with psychoses, met carriers of the BDNF val66met with high level of childhood abuse have more cognitive and brain abnormalities than all other groups.
https://pubmed.ncbi.nlm.nih.gov/23876786/
Let's translate. Basically, the type of BDNF variant a person had (less production of BNDF in this case) connected early trauma with later mental health issues.
This met version of BDNF leads to a reduced production of it and its effect on PTSD?
Specifically, the study revealed that the allelic frequency of BDNF met was twofold higher in those with probable PTSD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5742797/
What's the mechanism of this connection?
Changes in BDNF transcription is the major causal agent for the changes in spine density following stress.
https://www.sciencedirect.com/science/article/pii/S0301008213001160
Okay...so BDNF function directly drove how stress affected the actual brain structure and connectivity.
Most importantly, this was found in the hippocampus, the brain area intimately tied to trauma, memory, and mood.
BDNF-related neuroplasticity is considered an important component in maintaining the integrity of the hippocampus
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5742797/
In fact, BDNF during trauma may cause the increased fear response in the amygdala, our emotional control unit.
Remember...the brain is a prediction machine. If you experience a life-threatening event (or some degree of), the brain did not like the surprise and will ratchet up vigilance and fear to make sure it doesn't kill us the next time around.
That is the purpose of all the changes above! Be ready for the danger (even if it's not coming again).
This loop is what we're trying to break and BDNF is a key player in writing over the past connection.
Let's look at the flipside of trauma...addiction (usually the prescribed self-medication).
The two most common triggers for relapse?
- Stress
- Reduced BDNF levels
Goodness...might addiction just be the other side of the coin to trauma and its negative effects on the brain.
Look at the different things that are positive for trauma sufferers:
- Exercise - boosts BDNF in the brain
- Mindful meditation and Yoga - boosts BDNF (see meditation and neurogenesis)
- CBT - a slower version of using practice to guide BDNF and brain change
- Psilocybin - an explosion in BDNF
- CBD - directly boosts BDNF
Okay...we're showing our cards. Let's jump into CBD and psilocybin.
Research on CBD and trauma
We've covered a great deal on the pathways of trauma.
We have a full review of what exactly CBD is here so let's jump right into its effects on trauma.
Let's zero in on these facets with CBD:
- CBD and serotonin
- CBD and GABA
- CBD and inflammation
- CBD and stress response
- CBD and fear extinction
- CBD and BDNF
First, we'll start with the neurotransmitters at play.
CBD and serotonin for trauma
We looked at how serotonin lies at the intersection of stress buffer and repair (it drives BDNF).
Early trauma can affect serotonin function long-term as well.
CBD is very different from SSRIs which boost serotonin in one direction (see CBD versus SSRIs).
CBD acts as a feedback mechanism when it's depleted. Technically, it's called an allosteric positive modulator.
We have a great deal of research on our CBD and serotonin review.
A perfect example is a serotonin depleted due to pain:
repeated treatment with low-dose CBD induces analgesia predominantly through TRPV1 activation, reduces anxiety through 5-HT1A receptor activation, and rescues impaired 5-HT neurotransmission under neuropathic pain conditions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6319597/
- CBD reduced pain (analgesia)
- CBD reduced anxiety
- CBD "rescued" serotonin (5HT) function
Keep in mind that the brain doesn't decipher between physical and psychological pain in terms of how serotonin functions as a buffer.
The downside with SSRIs is that they build tolerance since the brain doesn't like outside interference that pushes key pathways in one direction.
This is the so-called Serotonin Discontinuation Syndrome. Do you mean withdrawals???
Serotonin has a large management role across dopamine (motivation and addiction) and our other neurotransmitters.
Let's look at the "excitability" dynamic now.
CBD and GABA for trauma
GABA is the calming agent in the brain and nervous system. The brake pedal.
We've gone deep into the role of GABA in various reviews:
- CBD and GABA for anxiety
- CBD and glutamate (its counterpart)
- CBD and anxiety
- CBD and panic attacks
- CBD and sleep
With GABA, it's also a feedback player which is why you don't have a steady decrease in nervous system activity like you do with benzos (see CBD versus benzos) or even alcohol (CBD versus alcohol).
CBD is showing up across the anxiety spectrum of issues as a result:
Preclinical evidence conclusively demonstrates CBD’s efficacy in reducing anxiety behaviors relevant to multiple disorders, including PTSD, GAD, PD, OCD, and SAD, with a notable lack of anxiogenic effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604171/
GAD is general anxiety disorder. PD is panic disorder. SAD is social anxiety disorder.
All share a common pathway with GABA and the amygdala (fear center) overexpression.
Sleep figures very strongly into GABA's pathway as well!
Here's where it gets interesting.
A study looked at CBD's effect on GABA between a control group and people with autism.
CBD had different effects:
Across regions, CBD increased GABA+ in controls, but decreased GABA+ in ASD; the group difference in change in GABA + in the DMPFC was significant.
https://www.nature.com/articles/s41386-019-0333-8
It's very unusual for a substance to have different effects on a common pathway depending on brain area and state!
The above makes sense when you understand that the prefrontal cortex in people with autism may be downregulated (running slow) and that more glutamate is actually what is needed there!
We see this same effect with dopamine and schizophrenia which actually has too much dopamine function in one area (striatum) but not enough in the prefrontal cortex.
See CBD and schizophrenia to look at those studies.
GABA and glutamate are base-level neurotransmitters needed in every neuron and it gets very complicated fast.
The beauty is that CBD buffers our endocannabinoid system which is tasked with balancing these systems.
One direction does not work in the brain!
Feedback is the way to go and that's CBD's greatest strength.
Let's turn to the immune system now.
CBD and inflammation for trauma
Trauma sets off an inflammatory storm in the brain that is highly destructive.
It's very important to calm the immune system's overheating before any healing can be done.
Abuse and other traumatic events (even social rejection) are no different than taking a hit to the head in terms of our brain's inflammatory response:
Neurobiological research is reconciling this conflict by suggesting that psychological trauma, and particularly childhood psychological trauma, can trigger the same physiological response as physical trauma
https://www.tandfonline.com/doi/pdf/10.1080/20008198.2017.1375840
It only knows one response!
You can even see the inflammatory markers in the blood:
We reported initial evidence of association between childhood maltreatment and high levels of several inflammation biomarkers in 1000 members of the Dunedin Multidisciplinary Health and Development Study, who were followed up from birth to age 32 years
There are two general types of inflammation we'll look at with CBD:
- Cytokines - inflammatory messengers
- Oxidative stress- highly destructive forms of oxygen
Let's look at actual examples.
First, the cytokines:
The level of IL-1β, MCP-1, and TNF-α increased over time in PTSD compared to non-PTSD patients
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6149900/
These are all markers of increased inflammation.
And CBD?
The levels of IL-4, IL-5, IL-13, IL-6, IL-10, and TNF-α were determinate in the serum. CBD treatment was able to decrease the serum levels of all analyzed cytokines except for IL-10 levels.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458548/
And MCP-1?
CBD significantly attenuated LPS-induced NF-κB activity and IL-8 and MCP-1 release from macrophages.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6917034/
Most interestingly, CBD will do this when inflammation is high but not when it's low. It can actually bolster immune response when low.
Check out CBD and neuroinflammation for much more info.
What about oxidative stress?
Let's compare it to the big anti-oxidants we all know of:
CBD exhibits much more antioxidant activity (30–50%) than α-tocopherol or vitamin C [4].
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7023045/
Goodness. Check out CBD and oxidative stress to learn more.
One interesting note...the effect of CBD is dependent on the state of the system:
- Healthy neuron with low oxidative stress - CBD has no effect
- Healthy neuron with high oxidative stress- CBD reduces oxidative stress
- Cancerous or virally infected neuron - CBD INCREASES oxidative stress
Three different responses but what's with the third one?
It mimics how our immune system naturally deals with wayward cells...it jacks up oxidative stress to kill the cell.
Chemo and radiation are basically massive amounts of oxidative stress.
Check out CBD and Turkey Tail for pathways of cancer.
Also, NAC is a powerful buffer for glutathione, our primary antioxidant.
Related: CBD and glutathione.
Let's turn to stress.
CBD and stress response for trauma
We looked at serotonin. What about cortisol and anandamide? Even corticotrophin-releasing factor?
First, the stress side...cortisol and CRF.
In one study on the effects of CBD, researchers found that cortisol levels decreased more significantly when participants took 300 or 600 mg of CBD oil
https://www.medicalnewstoday.com/articles/cbd-and-sleep
This was a sleep study that shows how important cortisol is to the sleep/wake cycle.
See CBD and cortisol.
What about the initiator of the whole stress response cascade? CRF.
Interestingly, cannabidiol at low (5 mg/kg) and intermediate doses (15 mg/kg) successfully blocked the effects induced by acute stress on corticotropin-releasing factor, pro-opiomelanocortin and glucocorticoid receptor gene expression.
https://pubmed.ncbi.nlm.nih.gov/30324842/
See CBD and CRF.
Let's turn to the response beyond serotonin.
Hello Anandamide!
CBD's effect on anandamide:
CBD also inhibits FAAH, which results in increased anandamide levels.
https://www.frontiersin.org/articles/10.3389/fphar.2018.00482/full
Just a reminder...
Accumulating evidence suggests that the eCB anandamide (AEA) promotes fear extinction [4] and protects against the anxiogenic effects of stress through the activation of CB1 receptors [5,6,7,8]
https://www.nature.com/articles/s41380-018-0215-1
Okay...the anxiety effects of stress are a big one but….wait a minute...fear extinction?
Let's get into this.
CBD and fear extinction for trauma
Fear extinction is literally the erasing of the hard-wired imprint of the original traumatic event.
This is both memory and emotional in nature.
Think of how water flows.
It will eventually carve out a stream and then a river. Literally cut through mountains of rock with time.
Repetitive action (chronic stress or low-level social rejection) will eventually get there. Trauma rips through the ground!
That's the basis behind CBT (cognitive behavioral therapy) - repetition to cause brain change and thus, behavior change.
With trauma that's significant, this process can occur in an instant.
Locked into brain architecture like writing the trauma in wet concrete.
Fear extinction is actually part of a broader process called neurogenesis...building new brain pathways and overwriting old ones.
CBD's effect there?
These findings provide the first evidence that CBD can enhance the consolidation of extinction learning in humans and suggest that CBD may have potential as an adjunct to extinction-based therapies for anxiety disorders.
https://secure.hawaiianethos.com/assets/resources/2013%20Das%20-%20CBD%20Fear%20Extinction.pdf
Animal studies have found that CBD can help individuals who are more prone to stress (remember, our stress system is imbalanced following trauma) with "forgetting" the original trauma.
Taken together, the present data indicate that enhancement of mGlu5 receptor signaling in populations vulnerable to stress may serve to offset a resistance to fear memory extinction without producing anxiogenic effects.
https://www.frontiersin.org/articles/10.3389/fnbeh.2019.00091/full
We would expect BDNF to be in pay with ANY change in the brain.
What about CBD there?
Cannabidiol Induces Rapid and Sustained Antidepressant-Like Effects Through Increased BDNF Signaling and Synaptogenesis in the Prefrontal Cortex
https://pubmed.ncbi.nlm.nih.gov/29869197/
Check out CBD and depression to learn why this is so important. We actually dug into how SSRIs really work (till tolerance kicks in) and it's mainly BDNF.
Again, serotonin drives BDNF (and ladies, estrogen drives serotonin - see estrogen and mental health).
The brain area noted is important as well...the prefrontal cortex.
Remember, this is the area that's tasked with rationally keeping our emotional and fear area (amygdala) under control.
In fact, trauma damages both that area and the connectivity between it and other brain areas.
This "connectivity" is mainly via white brain matter and that's a big difference between CBD and THC.
CBD promotes white matter volume while THC has been shown to actually hurt it.
See CBD is a must if you use THC.
Check out CBD and BDNF or CBD and brain repair to learn more.
Finally, we have a big review of CBD and traumatic brain injury which is important as many of the same mechanisms are at play (excess glutamate, inflammation, oxidative stress, BDNF and serotonin depletion, etc).
Let's turn to psilocybin.
Research on psilocybin and trauma
We have a massive review of psilocybin and mental health already.
Let's zero in on the two critical pieces of trauma that psilocybin directly affects:
- BDNF - neurogenesis
- Connectome reset
Okay, the first should be old hat by now.
Any kind of change in the brain (say...from a traumatic state) requires neurogenesis...building new pathways and forgetting old ones (fear extinction from above).
Psilocybin creates an explosion in neurogenesis!
serotonergic psychedelics are capable of robustly increasing neuritogenesis and/or spinogenesis both in vitro and in vivo.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082376/
Remember that serotonin drives BDNF….this is how SSRIs work till tolerance sends it the other way.
Interestingly for trauma (locked in memory state), the effects were very pronounced in the hippocampus so tied to trauma but not just there:
Extinction of "fear conditioning" may be mediated by actions of the drugs at sites other than hippocampus such as the amygdala, which is known to mediate the perception of fear.
https://pubmed.ncbi.nlm.nih.gov/23727882/
Trauma is a persistent state of "fear conditioning" for the original event. A constant state of vigilance so it doesn't happen again with surprise.
Psilocybin is able to unwind this!
This same effect applies to all the psychedelics but psilocybin's safety profile is much better.
Magnesium glycinate or L-Threonate is important to take with psilocybin as all this brain activity draws down mag.
Okay...that's the part which is shared with CBD...and exercise, and meditation, and CBT...but at much faster rates.
The other piece is revolutionary and psilocybin (plus psychedelics) may be the only way we know to get there.
Psilocybin and connectome reset
This is cutting-edge brain science now.
There are different brain states that we flip between as needed (if the brain is healthy).
Remember the Default Mode from above? Daydreaming. Ruminating. Our historical sense of self?
That state reflects a particular "highway" of connections across different brain areas.
It's very different than the other dominant state called Task-Positive mode.
This is when you're focusing on a particular problem...say directions on a map or math.
These states literally look different in terms of brain connectivity activity.
They're are called networks for that reason and the map of all connections and modes is called the connectome.
Alright...why bother with all this nonsense?
It wasn't till we have brain scans in real-time that we could even see these differences.
This is a very new science!
Inability to flip correctly between states is tied to various mental health issues including those that come from trauma.
Schizophrenia - literally stuck in default mode (see CBD and schizophrenia)
Hyperactivity of the default-mode network in first-episode, drug-naive schizophrenia at rest revealed by family-based case-control and traditional case-control designs
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5380243/
Anxiety and depression
The resting state brain networks, particularly the Default Mode Network (DMN), have been found to be altered in several psychopathological conditions such as depression and anxiety.
https://pubmed.ncbi.nlm.nih.gov/25804311/
Think about the entire collection of issues such as OCD, repetitive thoughts, and negative rumination.
These all indicate that fear is stuck in the "ruminating" network of default mode.
It's almost as if it's not in your conscious control and just runs in the background. That's Default Mode!!
A blurring of the lines between it and the task-positive mode. Stuck in limbo.
Okay...let's turn to trauma.
There's definitely an imprint of trauma on this connectome:
Results revealed that DMN connectivity was reduced in veterans exposed to combat trauma with and without PTSD compared to healthy civilian controls.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4810776/
Maybe more importantly:
Findings suggest that the experience of trauma, rather than the pathology of PTSD, may be related to DMN changes.
What about early life trauma?
Here, we propose that early-life trauma may interfere with the developmental trajectory of the DMN and its associated functions
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3004976/
Okay...let's put the pieces together...why does this matter...what's the big deal about the default mode?
Critically, developmental changes in the DMN may parallel those observed in other associated domains, including self-referential processing, autobiographical memory, prospection, and theory of mind
Goodness….the Default Mode governs how we look at ourselves, how we record the events that made us (including trauma), and literally our concept of "mind".
Take a minute to think about that. Our thinking selves are literally marbleized into the default mode and trauma disrupts it.
There's only one thing we have ever come across (as much as we love CBD) that appears to affect this structure.
Psychedelics like psilocybin.
New brain scans are finally teasing out the secrets of "ego dissolution", etc.
In particular, psilocybin decreased functional connectivity of the right claustrum with DMN and increased right claustrum connectivity with task-positive networks.
https://psychedelicreview.com/the-role-of-the-claustrum-in-the-psychedelic-experience/
The claustrum is an interesting little thin sheet of brain mass that appears to coordinate all sensory inputs into a cohesive state.
It gets more interesting.
The claustrum may be part of the toolkit for consciousness as born out by trauma studies:
Claustrum damage was associated with the duration, but not frequency, of loss of consciousness, indicating that the claustrum may have an important role in regaining, but not maintaining, consciousness.
Acute stress like with trauma can actually route parts of the brain tied to vigilance and threat detection more tightly to the claustrum:
comparing PTSD + DS to controls, we observed increased functional connectivity of the BNST with the claustrum
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6866500/
Goodness...fear is being hardwired into our consciousness as a result of trauma.
Psilocybin temporarily disrupts these established networks and patterns.
To sum it up on a detailed study with treatment-resistant depression:
The post-treatment brain changes are different from previously observed acute effects of psilocybin and other ‘psychedelics’ yet were related to clinical outcomes. A ‘reset’ therapeutic mechanism is proposed.
https://www.nature.com/articles/s41598-017-13282-7
A "reset" mechanism.
We're not aware of any other class of substances that can "reset" the broader brain connection patterns.
It's truly fascinating. A gift down here.
Check out our review of psilocybin and mental health to really dive into the research.
Let's look at practical questions.
How much CBD or psilocybin for trauma
For CBD, we actually have some good research on this front.
Studies show that peak neurogenesis (our desired goal) is at 300 mg daily for CBD.
Beyond that, it actually starts to decrease as other pathways kick in.
Remember that serotonin drives BDNF and that's our intended target.
Safety studies have tested CBD up to 1500 mg with very strong profiles and we looked at using CBD long-term here.
CBD doesn't build tolerance, it's not addictive, and does not affect blood panel attributes.
The biggest piece there is tolerance. It's really important that we don't just spike serotonin (or GABA) the way that SSRIs and benzos do or anandamide the way THC does!
See CBD versus SSRIs or CBD versus benzos to learn more.
As for psilocybin, there are two approaches (based on dried mushroom):
- A hero dose - tripping which is generally 2-3 grams (maybe as low a 1 gram)
- Microdosing - .1-.5 mg
Microdosing will not have the trip effect but the neurogenesis is present over time.
Use in studies is generally every 3rd day and magnesium glycinate or L-Threonate should be taken prior to any psilocybin use as the brain-building process is taxing.
Again, you can read the full review.
We don't have hard research on microdosing and the default mode reset as we have with tripping doses.
We'll look forward to further studies on that front.
Let's connect the dots though.
The reset is a big part of psilocybin's effect on mental health issues and we know there's a known tie between early trauma and later mental issues.
Initial studies have shown perceived improvements but larger studies are underway. Psilocybin is going to upend the mental health field (thanks John Hopkins).
A wave of medical setting psilocybin treatment will be coming online very soon and is already available in certain areas for full doses in a guided setting (very important).
On a side note, exercise, mindful meditation, and yoga all support neurogenesis. It is THE key to recovery from trauma.
Let's look at type.
What's the best CBD or psilocybin for trauma
For CBD, there are baseline requirements:
- From organically grown in hemp in the US at FDA registered farms
- CO2 processed
- 3rd party tested
- No THC (THC builds tolerance longer term)
- No pesticides
- No mold
- No heavy metals
- No bacteria
- No solvents
Our test results are at the top of every page.
Then there's the type of CBD...Isolate versus full-spectrum (see CBD isolate versus full spectrum).
All the research is on CBD isolate. That's why we focus there.
More importantly, roughly 40-60% of the population has histamine issues and that number goes up as we get older and for women.
We tried 3-4 of the biggest CBD brands and had side effects due to this histamine issue.
CBD isolate actually has been shown to calm histamine response and mast cell activation (see CBD and histamine).
Histamine is part of the inflammatory pathway (which is upregulated with trauma) and it eats up GABA in the brain!
Then, there's cost.
We price CBD at 2-3 cents per mg of CBD before discounts up to 50%. To get to 300 mg daily, this is mandatory and it's the lowest price we can find for quality CBD isolate with 3rd party testing.
For psilocybin, it's trickier since it's not legal at the Federal level.
We're seeing a pattern of legalization similar to cannabis with Colorado and Oakland leading the way.
With more and more information coming out with John Hopkins leading the way, it's a matter of time before it's legalized throughout the country. Many trials are under way now for mental health and addiction.
In a famous study of drugs by the English godfather of addiction, psilocybin was listed as the safest drug (with alcohol being the most destructive).
We can't recommend a source as of yet for psilocybin due to its legality.
Again, check out our full review.
Okay...if you made it this far, congratulations!
We've covered how trauma, even early in life, can leave its mark directly on our brain.
CBD and psilocybin have fascinating effects on the repair and rewrite process in the brain.
Everyone has something traumatic in the past (even in utero) with far-reaching effects across mental health and addiction.
Be well. Take care of each other. Take care of yourself.
Related Research
How the immune system is the future of mental health (with tools)
CBD and brain repair
CBD and PTSD
Supporting pathways of resilience
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.


















1 comment
There might be a “reset” mechanism in play with the recent research on Nitrous Oxide and severe depression. It certainly works a different way. https://medicine.wustl.edu/news/laughing-gas-relieves-symptoms-in-people-with-treatment-resistant-depression/