CBD versus SSRI for Homicidal and Suicidal Thoughts
This is off our beaten path but after our extensive review of CBD versus SSRI's for serotonin and anxiety, we couldn't just turn our back on it.
More importantly, when I was dealing with crushing perimenopausal anxiety, Lexapro was casually offered up to me.
About 20 days into it, I started to have suicidal thoughts.
It's hard to explain this to another person who hasn't been there.
Yes, there are many other side effects (stomach, no joy, flat affect, insomnia, etc) but out of nowhere...suicidal thoughts. We looked at the problem with SSRIs in detail.
I've long since weaned off of Lexapro (see CBD and weaning off of SSRIs) but the question nagged at me.
How can medication cause thoughts about ending one's life if you've never felt that before?
What strange quirk in the brain has THAT specific effect?
Maybe more importantly, what about homicidal ideation or thoughts.
That popped up in our review of SSRIs versus CBD.
Of course, that prompted us to look at the murders associated with SSRI use.
The timing of mass shootings and the advent of SSRI may just be a coincidence.
It's harder to say that for the demographics of the shooters though.
We'll look at that below.
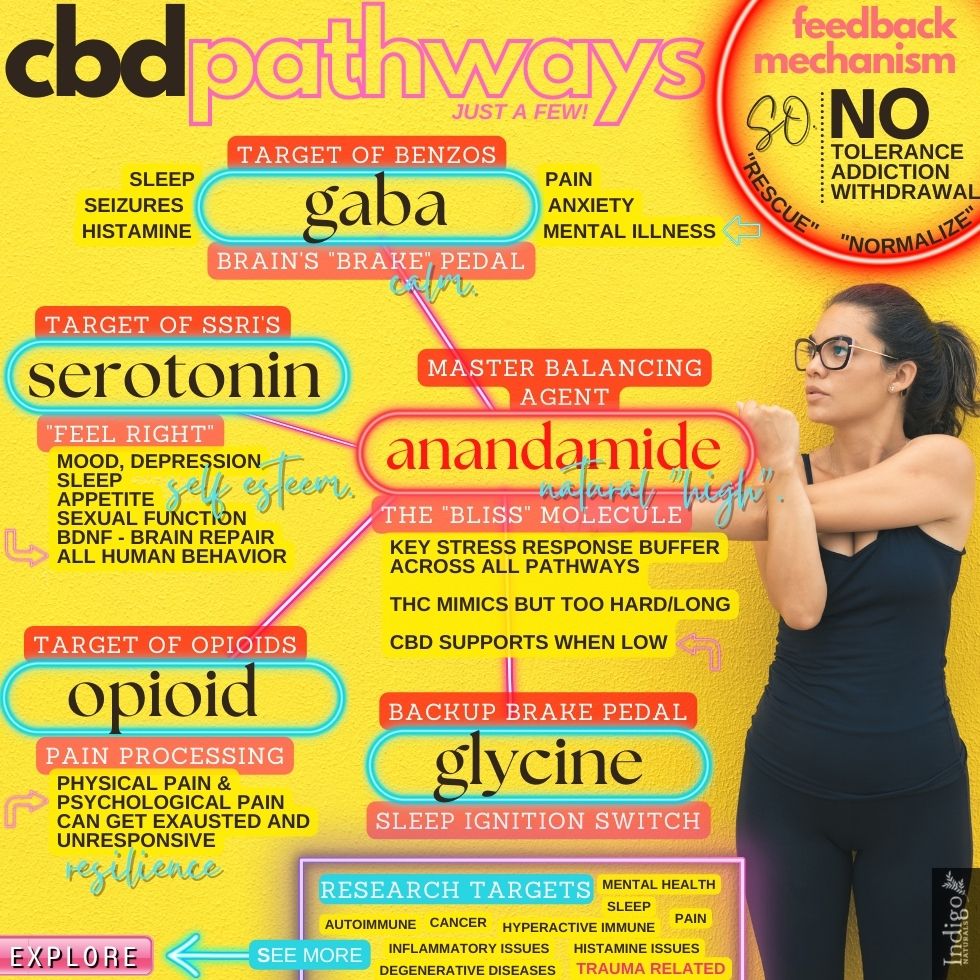
Since CBD works on the same serotonin pathways as SSRI's, is there a documented risk there as well?
If not, why not? Again, it's serotonin.
The topics we'll cover are as follows:
- How SSRI's work in the brain and body
- The history of SSRI's and homicidal or suicidal ideation
- Where does homicidal and suicidal ideation occur in the brain
- Who's at risk of homicidal and suicidal ideations from SSRI's
- Does CBD have the same risk?
Let's get started.
How SSRI's work in the brain and body
First, a quick recap.
SSRIs such as Lexapro, Effexor, Zoloft, and Prozac work by boosting the availability of serotonin in the nervous system.
Serotonin is a powerful workhorse neurotransmitter in the brain and gut.
In fact, most of our serotonin is made in the gut (hence all the gut-related side effects of SSRI's).
To say that serotonin is our "feel good" neurotransmitter is a simplification at best.
It's more than you can feel pretty terrible when it's too low, too high, or not functioning correctly.
SSRI's are primarily written for depression and anxiety (with less effect).
Researchers have teased out how SSRI's effect these pathways and THAT"S a fascinating story.
The quick summary is this…
SSRI's increase serotonin which boosts BDNF, our brain's fertilizer.
Check out CBD versus BDNF for more detail.
Essentially, for many (but not all), various insults can damage the brain's function:
- Chronic and acute stress
- Past trauma, especially during key points in brain development
- Immune system overreaction or infection
- Meandering foreign entities (bacteria) and chemicals
- Gut bacteria dysfunction
- Genetic variants in key genes
Serotonin and BDNF are key to the repair and rebuilding mechanism.
This is why people with depression or anxiety don't get immediate relief when taking SSRI's.
Even though the serotonin levels go up pretty quickly, it usually takes a few weeks to kick in.
Why?
Because neurogenesis (building a new brain) takes time!
In fact, they'll usually put you on benzos for these first few weeks since anxiety and depression can actually go UP during this initial time!
Here's the interesting piece.
Researchers would block neurogenesis and anti-anxiety/anti-depression effects go away.
They then block CB1 receptors (part of the endocannabinoid system where CBD operates), and the neurogenesis and anti-anxiety or antidepression effect of SSRI's is also blocked!
Again, check out the articles.
Like we said in the beginning, serotonin has its hands in many pies.
In fact, that's why it causes more anxiety/depression when boosted for the first few weeks.
It actually ramps up CRF (Corticotropin-Releasing Factor) which initiates our body's stress response.
Think fight or flight!
Check out CBD and CRF here.
The easiest way to see how widespread SSRI's operate in our nervous system and gut is to look at the side effects.
The full list of side effects.
For example, check out the list for Lexapro here:
https://www.webmd.com/drugs/2/drug-63990/lexapro-oral/details/list-sideeffects
- Inflammation of the nose?
- Giant hives?
And then…right after hallucinations...
Having Thoughts Of Suicide
Interestingly, homicidal ideation (having thoughts) wasn't listed there.
That's interesting since it's in NIH studies which we'll look at below.
Let's take a look at what we know on that front before diving into the brain to try to figure out what's going on.
The history and research of SSRI's and homicidal or suicidal ideation
Prozac came on the scene in 1987.
It was the birth of SSRI's, the most popular class of medications today for mental health issues.
Paxil (Paroxetine) followed in 1992.
Since then, we've had new additions with similar pathways.
First, we have to understand that depression is the leading condition that they're prescribed for.
When the FDA released its black box warning on suicidal thoughts, many people stopped taking it and it resulted in more suicides.
Obviously, severe depression is a huge risk there.
The effectiveness of anxiety is more in question, however.
The key takeaway is that SSRI's can reduce suicidal thoughts in some patients and increase them in others.
This would seem to point to an underlying deficit or normal level of serotonin since you can't really test for that prior to use.
That being said, let's look at what research does show for both suicidal and homicidal ideation.
Ideation just means the thought of ("just" isn't the right word)...not necessarily the action.
We're actually getting some more rigorous studies on the matter.
It's hard to parse out suicidal ideation as a result of a pre-existing depression for which the SSRI was prescribed versus as a result of the medication.
One large scale study from England provided some clarity here.
It essentially compared different medications for suicidal ideation and suicide on a large-scale population:
The adjusted OR estimates comparing amitriptyline, fluoxetine, and paroxetine each with dothiepin as the reference group were 0.83, 1.16, and 1.29, respectively
https://jamanetwork.com/journals/jama/fullarticle/199120
This points to the relative risk for paroxetine (Paxil) being statistically significant.
The risk appears to be tied to age (young) and gender (male).
Another study found the risk was higher for adolescents:
However, in children and adolescents (aged 6-18 years), antidepressant drug treatment was significantly associated with suicide attempts (OR, 1.52; 95% CI, 1.12-2.07 [263 cases and 1241 controls]) and suicide deaths (OR, 15.62; 95% CI, 1.65-infinity [8 cases and 39 controls]).
https://www.ncbi.nlm.nih.gov/pubmed/16894062/
This study looked at a similar pool of severely depressed children with or without drug treatment.
The risk for attempts was 52% higher than those not treated with medications.
In 2007, the FDA came out with further warnings for SSRI and suicidal or homicidal ideation.
It required daily monitoring:
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
https://www.bmj.com/content/358/bmj.j3697/rr-4
The sad fact is this...we have to look to Europe for impartial data.
Not that the US is hiding data but as our friend in agriculture likes to day, you don't look for something you don't want to find (referring to E.coli in fields).
Some data from that field:
We showed for the first time that SSRIs in comparison with placebo increase aggression in children and adolescents, odds ratio 2.79 (95% CI 1.62 to 4.81) (2). This is an important finding considering the many school shootings where the killers were on SSRIs.
https://www.bmj.com/content/358/bmj.j3697/rr-4
Those were based on an analysis of 70 different trials.
Almost 3 times the risk!
Let's separate out an SSRI used for a condition outside of depression since that's less difficult to separate.
Duloxetine (Cymbalta) can be used for incontinence (which seems like bringing a bazooka to a knife fight but…).
There were also more women on duloxetine who experienced a core or potential psychotic event, relative risk RR 2.25 (95% CI 1.06 to 4.81).
Again, the more pronounced risk appears to be younger people:
Among adolescents, a recent study found that SSRIs utilization significantly increased the risk of completed or attempted suicide [45] whereas, among adults, SSRI use significantly decreased the risk of completed or attempted suicide and, among people aged 65 or more years, the use of SSRIs had a significant protective effect [45].
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4034101/
That's not surprising based on how SSRI's actually work in the brain (brain repair mechanisms which decrease as we get older).
We see this over and over again:
Although exposure to SSRIs increased the risk of completed or attempted suicide among adolescents (odds ratio [OR] 1.92, 95% confidence interval [CI] 1.51-2.44), the risk was decreased among adults (OR 0.57, 95% CI 0.47-0.70).
https://www.ncbi.nlm.nih.gov/pubmed/19188627/
Then there's the comparison of SSRI's versus other antidepressants which helps to offset the initial probability of a depressive state:
A recent Canadian study27 reviewed coroners’ reports of suicides and found that patients treated with SSRIs were 5 times more likely to have committed suicide within the first month of treatment than patients treated with other antidepressants.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2464814/
Then there are studies for people where the state of suicidal ideation is tied to use of the medication and goes away after stopping:
Six depressed patients free of recent serious suicidal ideation developed intense, violent suicidal preoccupation after 2-7 weeks of fluoxetine treatment. This state persisted for as little as 3 days to as long as 3 months after discontinuation of fluoxetine. None of these patients had ever experienced a similar state during treatment with any other psychotropic drug.
https://www.ncbi.nlm.nih.gov/pubmed/2301661
Interestingly, treatment created a sudden and intense focus on suicide.
Another study on Swedish children (the Swedish system is able to track every patient and cross-analyze data because of this), found that risk for suicide with SSRI compared to placebo was much higher:
11% versus 2.7%.
Again, the underlying diagnosis was similar for the population so shouldn't SSRI's reduce suicide attempts versus placebo?
You can see popular SSRI's compared to placebo for suicidal thoughts and attempts here:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC193979/table/t1-2/?report=objectonly
And again, to rule out the underlying depression diagnosis:
For instance, in Pierre Fabre's clinical trial database of approximately 8000 patients, the rate for suicidal acts by those taking SSRIs appears to be 3 times the rate for other antidepressants
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC193979/
We'll look at important demographic differences below which help to explain some conflicting studies on this front (which manufacturers are quick to point to).
Let's look at the other side which is pressing against today's headlines of mass shootings.
Homicidal ideation and SSRI
What on earth is going on there?
First, let's look at the "ideation" or thoughts part of it.
What does the research show?
First, let's look at history and studies of course.
An interesting turn occurred on this front when the British government required data from GlaxoSmithKline, the manufacturer of paroxetine (generic for Paxil).
The summary:
In these trials, hostile events are found to excess in both adults and children on paroxetine compared with placebo and are found across indications, and both on therapy and during withdrawal.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1564177/
"Hostile events" was the umbrella term by GlaxoSmithKline for the following:
homicide, homicidal acts, and homicidal ideation as well as aggressive events and “conduct disorders”
Analysis by type of SSRI is helpful as it helps to weed out general depressive underpinnings:
There were three for fluvoxamine, four for citalopram, 10 each for paroxetine and sertraline, and 31 for fluoxetine.
http://psychrights.org/research/Digest/SSRIs/kauffman2009.pdf
Maybe more interesting was the result of paroxetine on healthy individuals (no depression diagnosis):
Finally, in healthy volunteer studies, hostile events occurred in three of 271 (1.1%) volunteers taking paroxetine, compared with zero in 138 taking placebo
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1564177/
Again, it's important to parse out depression itself although this is less important with homicidal ideation than for suicidal ideation.
What about the newer class of SSRIs like Lexapro, Effexor, or Zoloft?
Here's a sample for sertraline (Zoloft):
In these trials, eight of 189 patients randomized to sertraline discontinued for aggression, agitation, or hyperkinesis (a coding term for akathisia), compared with no dropouts for these reasons in 184 patients on placebo (95% CI, 1.72–infinity).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1564177/
That was a pediatric study which is important as we'll see later.
Here's data by type of SSRI:
Prozac (fluoxetine) was most commonly linked to aggression, increasing violent behavior 10.9 times. Paxil (paroxetine), Luvox (fluvoxamine), Effexor (venlafaxine) and Pristiq (desvenlafaxine) were 10.3, 8.4, 8.3 and 7.9 times, respectively, more likely to be linked with violence.
https://www.livescience.com/32934-do-antidepressants-increase-violent-behavior-111102html.html
What about the class of SSRI drugs in their entirety?
Let's look at medications across the entire market to see if the class itself stands out.
First…
We identified 1527 cases of violence disproportionately reported for 31 drugs. Primary suspect drugs included varenicline (an aid to smoking cessation), 11 antidepressants, 6 sedative/hypnotics, and 3 drugs for attention deficit hyperactivity disorder
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0015337
Their conclusion in case it's not obvious:
Varenicline, which increases the availability of dopamine, and antidepressants with serotonergic effects were the most strongly and consistently implicated drugs.
So the class itself has an issue among all the medications on the market for any issue.
Five SSRI's stood out on the list:
Prozac (fluoxetine) was most commonly linked to aggression, increasing violent behavior 10.9 times. Paxil (paroxetine), Luvox (fluvoxamine), Effexor (venlafaxine) and Pristiq (desvenlafaxine) were 10.3, 8.4, 8.3 and 7.9 times, respectively, more likely to be linked with violence.
https://www.livescience.com/32934-do-antidepressants-increase-violent-behavior-111102html.html
The Japanese Ministry of Health followed with a warning after studying the link between SSRI's and violence:
"There are cases where we cannot rule out a causal relationship [of hostility, anxiety, and sudden acts of violence] with the medication."
https://www.medicalnewstoday.com/releases/151688.php
There a long list of specific acts of violence and mass violence where the perpetrator was on SSRI's, SNRI's and anti-psychotic medications.
https://SSRIstories.org
https://www.cchrint.org/pdfs/violence-report.pdf
https://www.zerohedge.com/news/2019-05-18/prescription-violence-corresponding-rise-antidepressants-ssris-mass-shootings
A book really gets into the history and detail of SSRI and suicide or homicide here.
It's not happy reading.
But SSRI's are incredibly successful, right?
There's a great review of 1000's of trials on this front.
While only half of these trials had formally significant effectiveness, published reports almost ubiquitously claimed significant results. "Negative" trials were either left unpublished or were distorted to present "positive" results.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2412901/
It appears that they were more successful based on the severity of depression and this skews the overall data (if you're looking to "expand" the benefits and market).
Drug-placebo differences increased with increasing baseline severity and the difference became large enough to be clinically important only in the very small minority of patient populations with severe major depression.
This was more a play with the placebo:
In severe major depression, antidepressants did not become more effective, simply placebo lost effectiveness.
Of all the studies we looked at, that may be the most interesting analysis of why SSRI's are the most popular class of prescribed medications with over 30 million Americans on them.
You can find all this information across various NIH studies online and much more. This is a small smattering of studies out there.
That's where most sites end but as you may have noticed in our review of CBD versus SSRIs or CBD versus anti-anxiety meds, we like to go deeper.
What do we know about the mechanism of suicidal and homicidal ideation?
We're not talking about the results of being severely depressed but the sudden thought of suicide or homicide that can occur with SSRI.
Where is THAT??
Where does homicidal and suicidal ideation occur in the brain
First, there are some studies surrounding specific genes and this risk from treatment specifically (as opposed to general suicidal thoughts):
We have previously described the association between treatment-emergent suicidal ideation (TESI) and markers in genes encoding the glutamate receptors GRIK2 and GRIA3
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2819190/
Glutamate is the brain's gas pedal (as opposed to GABA).
So, perhaps ramping up activity but in a way (or area) that leads to these thoughts.
We'll look at that.
They also found two other genes:
These markers reside within the genes PAPLN and IL28RA, respectively.
These get a little more technical but the latter deals with the immune system (see CBD and neuroinflammation).
The glutamate angle is interesting since there is a tie with it's opposing force (the "brake") GABA for suicide.
Poulter and his colleagues found that one of the thousands of types of receptors for GABA is underrepresented in the frontopolar cortex of people with major depressive disorder who have committed suicide as compared with nondepressed people who died of other causes.
https://www.scientificamerican.com/article/the-origins-of-suicidal-brains/
That link is an interesting read as it talks about epigenetic changes from early abuse and trauma.
Epigenetics just means how genes are turned on and off by our environment (and even our mother's womb, ancestors, etc).
Even in the womb, epigenetic influences can change the developing brain in ways that increase the risk of eventual suicide
And finally, the relevance for SSRIs potentially:
The researchers, publishing in the Journal of Epidemiology and Community Health, suggest that the chemical serotonin, which is involved in fetal brain growth, may play a role.
They showed that reduced serotonin was at play here.
We've covered CBD and serotonin or CBD and BDNF (the big builders of the brain) extensively since they can play a key role in anxiety and depression.
Now, that's reduced serotonin where SSRI's boost serotonin.
Disrupting such a critical system can have varied results across all the different genetic profiles.
Another study found a connection directly with a serotonin gene:
Association of polymorphism of serotonin 2A receptor gene with suicidal ideation in major depressive disorder
To sum it up:
The 5HT1A receptor may be crucial to the whole suicide process and also play a role in the neural circuitry affecting mood regulation and decision-making.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4649802/
5HT is the serotonin pathway.
Let's look quickly at Serotonin Syndrome which is having too much serotonin.
One note...when you are given a prescription for SSRI, this is based on a test that shows your serotonin levels are too low.
NOT!!!
They can't accurately test for serotonin.
The prescription is made purely on the basis of symptoms of depression (or anxiety or a catch-all of mental health issues).
As we looked at CBD for perimenopause depression, there are many factors that can figure into depression (hormones, overactive immune response, inflammation, stress, trauma, poor rebuilding pathways, etc).
A good percentage of people with depression may have adequate serotonin levels.
Now, their GP is going to write a script for a medication that will boost those levels.
A percentage of those people will now have excessive serotonin levels and get Serotonin Syndrome.
A retrospective cohort study reviewing Veterans Health Administration records from 2009–2013 showed a disease incidence of 0.23% in patients exposed to serotonergic medications
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6539562/
.23%. That's not too bad.
What's .23% of 30,000,000 (estimated SSRI users in the US)?
69,000.
A study from GlaxoSmithKline (manufacturer of paroxetine) showed a much higher percentage for "hostile events":
When hostile events occurring in both adult and pediatric trials are summed, both on therapy and during the 30-day drug-free phase after taper had finished, 60 (0.65%) of 9,219 patients overall had hostile events
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1564177/
That's almost 2 million people in the US and that's from the manufacturers (would love impartial, "un-scripted" study results).
What are some attributes of Serotonin Syndrome?:
Cases were reported by as many as 12 different investigators, and the most commonly reported symptoms included confusion (n = 16), hypomania (n = 8), restlessness (n = 17), and myoclonus (n = 13)
Hypomania and restlessness.
Hypomania is a mildly manic state.
I actually ran from that state after the initial prescription to the opposite after 1-2 weeks.
Feeling very flat with no emotional affect.
I felt that personally from Lexapro. Nothing tasted good. Nothing sounded good. Just...flat.
Apparently, I'm not alone:
As for prevalence rates, according to a study by Bolling and Kohlenberg,9 approximately 20 percent of 161 patients who were prescribed an SSRI reported apathy and 16.1 percent described a loss of ambition.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2989833/
Their description:
The preceding authors also describe a number of distinct emotional themes in affected patients, including a general reduction in the intensity of experience of all emotions, both positive and negative; a sense of emotional detachment; “just not caring;”
Emotional detachment. Put a checkmark next to that one for later.
Like we said, serotonin has its fingers in many pies!
Just check out this chart for escalating symptoms for Serotonin Syndrome:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6539562/figure/ijms-20-02288-f001/
To see the extreme, it can even cause tardive akinesia.
What's that?
Tardive dyskinesia (TD) is a disorder that results in involuntary, repetitive body movements. This may include grimacing, sticking out the tongue, or smacking the lips.
Then there's restlessness...too much activity (glutamate).
Myoclonus is involuntary jerking motions (think of when you're falling asleep sitting down and jerk awake).
Now combine feeling totally flat (no joy) and coming out of your skin (restlessness).
Just a head's up...the one big warning you will get is that it's hard or dangerous to come off of SSRI's. (see CBD to wean off SSRI's).
Work with your doctor and be very careful. Again, any shifting of this apple cart is like chemical surgery on your nervous system (which begs the question).
Withdrawal from antidepressant medications may also be mistaken for SS (Serotonin Syndrome). Antidepressant withdrawal syndrome is typically associated with second-generation antidepressants
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6539562/
Remember, Serotonin Syndrome is the extreme version of too much serotonin but side effects from just elevated levels are equally varied.
Back to side effects of SSRI's…
You can see very different effects depending on the person:
It is well-known that antidepressant treatment is associated with over-stimulation, restlessness resembling akathisia, agitation, insomnia, severe anxiety, mixed-dysphoric bipolar states, or psychosis in some patients
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4034101/
The bipolar states and SSRIs are a known risk to the point that the FDA issued a strong warning.
In fact, there's a strong association when a person is in a hypomanic state:
Clinicians should assess Intra-MDE racing/crowded thoughts and psychomotor agitation, as antidepressants alone may worsen these symptoms, and this may induce or increase suicidal behavior.
intra-MDE is code for hypomania periods between depressive states.
Why this warning?
Suicidal ideation was present in 52.6%.
https://www.ncbi.nlm.nih.gov/pubmed/15532094
That's a great segue into homicidal ideation and SSRI links (unfortunately).
There's some interesting new research.
One study looked at variations in a specific gene tied to violence from SSRI's.
Essentially, people with a mutation in a liver processing pathway that breaks down SSRIs and/or serotonin may lead to a build-up:
Antidepressant-induced akathisia-related homicides associated with diminishing mutations in metabolizing genes of the CYP450 family
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3513220/
There's that akathisia - known side effect with SSRI use.
What is akathisia again?
It’s a torturous condition where the sufferer feels an incredible, irresistible restlessness. The feeling creates constant, repetitive movements like pacing, rocking back and forth, or swaying.
https://www.medprodisposal.com/akathisia-15-things-to-know-about-this-horrible-condition/
Think of your worst caffeine irritability and ratchet that up to 10.
It's very common with withdrawal states for methamphetamine, alcohol, and other drug withdrawals.
Increased violence is associated with mental health usually in the additional context of substance abuse.
Bi-polar (including hypomania) is one of the bigger examples of this.
Back to akathisia...some known symptoms (focus on the second to the last one):
- A sense of extreme, irresistible restlessness
- Irritability
- Panic
- Tension
- Agitation
- Anxiety
- Emotional unease
- Insomnia
- Dark, unpleasant thoughts
- Impatience
Akathisia can also sometimes lead to violent, aggressive impulses or suicide. Sufferers often can’t pinpoint the source of their distress, though it can feel unbearable.
https://www.medprodisposal.com/akathisia-15-things-to-know-about-this-horrible-condition/
As for SSRI's:
Patients taking these drugs have a 20% chance of suffering from akathisia symptoms.
Interestingly, we can look at other classes of drugs that are associated with homicidal thoughts and violence.
Neuroleptics (a class of antipsychotics) are serious tranquilizers.
The development of akathisia as a parkinsonian side effect is confirmed in the use of these drugs.
https://jamanetwork.com/journals/jama/article-abstract/362208
Then there are known adverse effects of metoclopramide, which is used for gut issues.
Most of our serotonin is made in the gut and it plays a key role there.
For example, a case study with this drug:
The adverse effects of agitation and homicidal ideation were temporally related to the starting and stopping of metoclopramide.
https://www.ncbi.nlm.nih.gov/pubmed/21907057
That's odd.
What are the side effects of metoclopramide?:
Common side effects include: feeling tired, diarrhea, and feeling restless. More serious side effects include: movement disorder like tardive dyskinesia, a condition called a neuroleptic malignant syndrome, and depression
https://en.wikipedia.org/wiki/Metoclopramide
Wait, what?? dyskinesia??
This is a popular anti-nausea drug and granted, that's a one-off example...but the shared side-effects are interesting.
Metoclopramide works primarily on dopamine function and...wait for it….serotonin function!
On a side note, I was prescribed this drug for (brand name is Reglan) at ER visit for nausea following perimenopause.
Apparently this is a known no-no (severe contraindication technically) with SSRI's (like the Lexapro they knew I was on).
Needless to say, I had a psychotic break, severe suicidal thoughts, and dyskinesia (chattering of teeth, legs jerking around, etc).
It was the worst night of my life. Bar none. Serotonin syndrome.
Onward!
Again...this wild study looked at akinesia and resulting violence:
Both victims and assailants were akathisic before about half of all incidents; bystanders rarely were.
https://www.ncbi.nlm.nih.gov/pubmed/1973544
Speaking of dopamine… there's psychosis and SSRI's
When you look through all the examples (thousands) of mothers on SSRIs that murder their children or other horrific examples, many say they were in a stupor or don't remember what happened.
Like a dream. Nightmare, really. They are generally horrified and wrecked by remorse.
Is there a tie between SSRI's and psychosis?
A University looked at admissions data and found:
Forty-three (8.1%) of 533 patients were found to have been admitted owing to antidepressant-associated mania or psychosis.
https://www.ncbi.nlm.nih.gov/pubmed/11235925
Oh but it's a small number.
Technically, the number of mass-shooters and homicides referenced at ssristories.com is small as well.
Excessive dopamine has been tied to psychosis states but this is the brain after-all. Nothing's easy.
The results suggest abnormal levels of the neurotransmitter glutamate may lead to changes in the levels of another neurotransmitter, dopamine, causing the transition into psychosis.
https://www.livescience.com/35009-brain-chemicals-cooperate-to-cause-psychosis-study-suggests.html
We'll actually touch on CBD and schizophrenia below which is fascinating for balancing key brain messengers.
Although the effect of antidepressants shows with homicides, benzos and opioids may be an even bigger issue (see CBD versus benzos for GABA):
The analysis based on case-control design showed an adjusted OR of 1.30 (95% CI: 0.97-1.75) as the risk of homicide for the current use of an antidepressant, 2.52 (95% CI: 1.90-3.35) for benzodiazepines, 0.62 (95% CI: 0.41-0.93) for antipsychotics, and 2.16 (95% CI: 1.41-3.30) for opioid analgesics.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4471985/
The uncontrollable movements of Serotonin syndrome remind us of OCD (see CBD and OCD here).
One study found a fascinating tie with OCD, violent thoughts, and suicidality:
Total OC symptom severity, unacceptable thoughts, and especially violent obsessions exhibited significant positive zero-order correlations with suicidality.
https://www.ncbi.nlm.nih.gov/pubmed/27659199
That is a good jump-off point for our next section.
Who's at risk of homicidal and suicidal ideations from SSRI's
Part of the issue or scapegoat for manufacturers is that different studies would show different results.
Remember how there are 1000's of SSRI trials and roughly 1/3rd do not get published.
The risk for suicide and homicidal ideation becomes more prevalent when you look at demographics:
Stratification by age showed that for the primary endpoint of suicidal ideation or behavior, for 18- to 24-year-olds, the risk was increased with medication compared with placebo, and the risk approached significance (OR = 1.62; 95% CI, 0.97, 2.71); for adults aged 25 to 64 years, the risk was significantly decreased (OR = 0.79; 95% CI, 0.64, 0.98); and for geriatric patients, the risk was markedly decreased (OR = 0.37; 95% CI, 0.18, 0.76) with antidepressants relative to placebo.
So...younger people showed a much higher risk than older people.
Here's the really important piece:
The rates were highest in children with obsessive-compulsive disorder (OCD), where the odds ratio of a hostile event was 17 times greater (95% confidence interval [CI], 2.22–130.0).
17 times greater!
OCD appears to have a major connection.
Excess glutamate (not enough GABA) is tied to a host of mental health issues with "excessive" activity:
Anxiety, OCD, ADHD, Parkinson's….dyskinesia!
Check out CBD and OCD to learn more.
GABA was introduced for patients with the most severe form of dyskinesia:
Tardive dyskinesia was significantly reduced, and preexisting parkinsonism increased slightly.
https://www.ncbi.nlm.nih.gov/pubmed/6108751
A separate pediatric study on sertraline showed a separately large risk for young people:
When discontinuations for any manifestation of treatment-induced activation (suicidal ideation or attempts, aggression, agitation, hyperkinesis, or aggravated depression) were considered, there were 15 discontinuations on sertraline compared with two on placebo, a relative risk of 7.3 (95% CI, 1.70–31.5; p = 0.0015).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1564177/
This risk of 7.3% is much lower than the 17% from younger people with OCD.
Another analysis of 850,000 people showed this same trend:
The “hazard ratio” for the 15-24 age group was 1.4 which roughly translates into a 40% increased likelihood.
The 15-24 range is fascinating as that's the key thrust of brain development during puberty.
Happenstance?
We think not.
As we learned from our wonderful perimenopause experience, times of hormonal flux are incredibly disruptive!
Also, there's another interesting factor.
Dyskinesia can actually pop up but not from medications.
A particular fact on its trajectory:
The disorder usually peaks in puberty and wanes or even abates during adulthood.
https://www.sciencedirect.com/topics/neuroscience/dyskinesia-syndrome
Goodness!
This all needs to be worked out by researchers but a possible pathway.
Dyskinesia is a disorder primarily of the subthalamic nucleus, an ancient part of the brain.
Here are some very curious facts about this area:
As one of the STN's suspected functions is in impulse control, dysfunction in this region has been implicated in obsessive-compulsive disorder
https://en.wikipedia.org/wiki/Subthalamic_nucleus
One STN regulator is the serotonin (5-HT) system.
https://www.ncbi.nlm.nih.gov/pubmed/24717335
Deep brain stimulation of this area for tardive dyskinesia is effective:
https://www.ncbi.nlm.nih.gov/pubmed/29433807
This area is mainly excitatory with glutamate neurons
https://www.ncbi.nlm.nih.gov/pubmed/24717335
So….let's recap.
We have a master control area with ties to OCD, dyskinesia, and serotonin.
The main risk for SSRIs and violence (suicide or homicide) appears to be for people age 15-24 with a pronounced risk with OCD (in fact, that's now part of SSRI warnings).
Hmmm.
Finally:
In contrast, local application of 5-HT or selective serotonin reuptake inhibitor (SSRI) administration excites most of GPe neurons
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3955837/
GP is a Global Pallidus which works with the subthalamus hand in hand.
Too little activation in this area can be Parkinson's. Too much??
They actually stimulate this area for Parkinson's and an unintended consequence:
Deep brain stimulation (DBS) of the subthalamic nucleus (STN) in particular is highly effective in relieving symptoms of Parkinson's disease (PD). However, it can also have marked psychiatric side effects, including delirium, mania, and psychosis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3589868/
Psychosis, mania, and delirium. Two of those showed prominently for suicidal and homicidal ideation (and acts).
It gets more interesting when they actually specify the outcomes from stimulating this area:
In patients with Parkinson's disease, subthalamic nucleus deep brain stimulation can occasionally induce mild personality changes, disinhibition, mood changes, hypersexuality and pathological gambling (Temel et al., 2005), ultimately influencing moral behavior.
https://academic.oup.com/brain/article/135/7/2006/350263
Ummm….relevant to the current spate of mass shootings?
Here's why we bring all this up.
Remember how SSRIs can actually increase anxiety and depression in the first few weeks of use?
Most doctors will prescribe benzos for this period saying that "it takes time for the SSRI to kick in".
That's either dishonest or born out of ignorance.
SSRI's can actually INCREASE anxiety/depression and the benzo is there to mask this increase.
Why on earth would it have this effect if it's so good for either condition?
Serotonin is EVERYWHERE in the brain.
It also controls the Corticotropin-Releasing Factor pathway.
That's our primary fight or flight circuit hormone between the body and brain.
During the initial period, SSRIs boost serotonin in this area as well which creates a heightened sense of anxiety, fear, and even depression.
See...you can't selectively increase serotonin by brain area.
What if SSRI's are boosting serotonin levels in the subthalamic nucleus (as appears to be the case from above) in people who already have higher activity there (dyskinesia, adolescents, OCD sufferers)?
We would love to see studies on people with Parkinson's' (too little subthalamic activity) who take SSRIs.
Until then...we wait for research to catch up.
What about CBD? Is the same risk there?
Does CBD have the same risk?
We've covered how CBD operates on the same serotonin pathways and that speaks to much of its anti-anxiety and anti-depressive effect.
A general review is at CBD and the mechanisms of anxiety here (they are varied after all).
What about the suicidal and homicidal ideation risk with SSRI?
We can't find and documented cases of suicidal or homicidal ideation in the research literature for CBD.
We need to clarify first.
This is for CBD isolate, by itself. Not THC or cannabis.
Both THC and cannabis can be associated with temporary states of psychosis (see CBD versus THC here).
CBD actually shows an opposing effect as is evident by research with schizophrenia and psychosis.
CBD was actually shown to normalize brain activity in people deemed pre-psychotic.
Read more about that at CBD and schizophrenia.
What about its effect on serotonin since that seems to be a key (if not sole) player in the SSRI effect.
Interestingly, CBD works with the endocannabinoid system we all have in our bodies.
This system is tasked with balance or homeostasis of other key systems:
- Nervous system - neurotransmitters including serotonin, GABA, Glutamate and more
- Endocrine system - hormones such as CRF, cortisol, and others
- Immune system - inflammatory agents and responders
First, serotonin.
CBD doesn't boost serotonin in one direction or we would see serotonin syndrome at much higher doses.
All over the research, you'll see words like "Modulate" or "normalize".
For example…
Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6319597/
We see the same thing with GABA (calms down glutamate activity).
Benzo's primarily increase GABA. They keep increasing GABA levels as doses go up along this trajectory:
- Calm
- Drowsy
- Amnesiac
- Hypnotic
- Anesthetic
- Death
An increasing slowing of activity until activity stops!
CBD affects GABA but within a range since the endocannabinoid system is about balancing.
There's no reported overdose of CBD for this reason (don't look up benzo stats...it's depressing).
That's actually an interesting sidebar here:
Preclinical evidence suggests that one aspect of the polypharmacy of CBD is that it modulates brain excitatory glutamate and inhibitory γ-aminobutyric acid (GABA) levels, including in brain regions linked to ASD, such as the basal ganglia (BG) and the dorsomedial prefrontal cortex (DMPFC).
https://www.ncbi.nlm.nih.gov/pubmed/30758329
There's that word, "modulate". Not boost or decrease. Balances!
Remember how too much glutamate and too little GABA were tied to the restlessness (akathisia) mentioned above?
Also, did you notice the brain areas they studied?
The basal ganglia. The subthalamus we spoke of before is directly tied to this area.
One note...CBD and SSRI's can use the same liver pathway for processing.
We want to make sure to work with your doctor and take them at least 4 hours away. Work with your doctor or naturopath for any supplement!
If the liver is busy processing CBD, it may boost or lessen the effect of the SSRI depending on its metabolism.
Check out CBD and OCD, CBD and unwanted thoughts, and CBD and depression for more information.
Finally, all our research is based on CBD Isolate.
That's why we only focus on Isolate.
As you can see, we don't mess around with research.
Also, be extremely careful if coming off of SSRI's. All the risks above can show on coming off or changing dosages/SSRI's.
We went through how we weaned off SSRIs with CBD here.
Be well. Be informed.
Be well. Take care of each other. Take care of yourself.
Related Research:
The Problem with SSRIs
CBD versus SSRIs
Top 10 Tips to Taper SSRIs
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.