Research on CBD and Perimenopause Anxiety

This is what started it all.
We're now dozens of intensive reviews into CBD and everything anxiety.
From BDNF to Social Anxiety to Fear of Flying.
Dozens of articles and 100's of NIH studies.
It all started, however, with an intense 24/7 anxiety as the result of perimenopause.
That story is here.
This wasn't a fearfulness but an overwhelming panic-like response.
There were signs of it a few years before.
A panic attack at a PTO meeting. Another weird response with a nurse at a doctor's office (would become full-blown white coat syndrome - see CBD and health anxiety).
In hindsight, it correlated with changes in my period and other little signals that something wasn't quite right.
I had never had anxiety though so this sudden and overwhelming change was frightening to me.
Needless to say, that does nothing to help the underlying anxiety!
We'll look at the usual approach most doctors have and how that almost ended me (literally).
We're going deep into this so hopefully women can avoid my "exploration".
The topics we'll look at:
- A quick refresher on the mechanism of anxiety
- Why anxiety hits women more than men
- Why does perimenopause cause anxiety
- Does perimenopause anxiety go away
- The standard medical approach for anxiety during perimenopause
- The endocannabinoid system and perimenopause anxiety
- Can CBD help with perimenopause anxiety
- Other supplements for perimenopause anxiety
- How much CBD to take for perimenopause anxiety
- What's the best CBD for perimenopause anxiety
Let's get started. We only have a few years to figure this out (please make it shorter!!).
A quick refresher on the mechanism of anxiety
We'll look at this circuit before jumping into the specific effects of hormones.
Anxiety doesn't just happen during perimenopause of course.
The anxiety "circuit" is pretty well established especially with new research.
You can learn all about it at our CBD and benefits for anxiety or CBD and the mechanism of anxiety.
The second item is more relevant for perimenopause as it speaks to effects that build with age!
A quick introduction to your brain!
There are three main areas to focus on:
- Amygdala - our emotional and fear processing area can be too strong
- Prefrontal cortex - our rational constraint and opposing force to the amygdala can be too weak
- Hippocampus - vulnerable "switch" for anxiety can be impaired
Yes, there are all sorts of other actors in play:
- Hormones (obviously the big target for perimenopause anxiety)
- Neurotransmitters like GABA and Serotonin (happen to be the targets for anxiety meds)
- Gut health - the new frontier
- Immune response - the newer frontier in mental health
Throw into this prior infection, trauma, stress (chronic and acute), and genes.
Lots at play here.
Some of these (neurotransmitters) speak to the feeling of anxiety RIGHT NOW!
Others are long term players that slowly emerge as...anxiety.
Check out CBD and long term anxiety for that piece.
Don't worry about remembering all this...we'll introduce them as needed below for perimenopause.
Before we get to that section, let's look at some clues that have to deal with gender.
Of course, we'll get into hormones because let's face it...that DRIVES perimenopause!
Just one more burden we have to bear!
Why anxiety hits women more than men
Before we introduce the hurricane that is perimenopause, we need to look at anxiety risk for women in general.
Is it different than for men? If so, why?
It's pretty well established that anxiety hits women quite a bit more than men:
The National Comorbidity Survey (NCS; conducted from 1990 to 1992) found that lifetime prevalence rates for any anxiety disorder were 30.5% for women and 19.2% for men
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3135672/
That's a 60% higher risk!
This was across the range of anxiety-related issues:
Prevalence rates were also higher in women than men for each anxiety disorder examined, including panic disorder (PD; 5.0% vs. 2.0%), agoraphobia (AG; 7.0% vs. 3.5%), specific phobia (15.7% vs. 6.7%), social anxiety disorder (SAD; 15.5% vs. 11.1%), generalized anxiety disorder (GAD; 6.6% vs. 3.6%; Kessler et al., 1994), and posttraumatic stress disorder (PTSD; 10.4% vs. 5.0%;
Why?
Here's the sad truth...there's not a lot of research on the mechanics behind the gender differences.
Big shocker.
There are two camps:
- Physical and neurological differences
- Social stress differences
- It's probably a blend of the two with hormones figuring strongly into the first.
Wait till you see how powerful our hormones are on the anxiety circuit.
Women going through perimenopause will issue a collective "duhh".
The second is more interesting.
Psychosocial stress differences.
Basically, women are stretched too thin and/or not happy with their roles in society.
That's obviously above our paygrade here but my gut says it speaks to why the birth rate is dropping significantly.
Women just don't want to take on so much stress.
As the mother of two teenagers, I can tell you it's overwhelming doing this during perimenopause.
I'm not alone.
As for one example of the importance of this social effect, the biggest disparity in age of onset for anxiety was between men of European descent and African American women.
Both gender and race figured into this equation here.
Psychosocial pressures.
Interestingly, social anxiety disorder does not show significant differences by gender of all the various diagnoses.
Let's look at neurological differences by gender for anxiety.
It may come down to stress response systems!
Brain scans looked at how men and women responded to stressful situations (the fearful face experiment is commonly used).
There were marked differences:
A gender-specific neural activation model underlying the central stress response has been observed in these studies. This includes asymmetric prefrontal activity in males and, primarily, limbic activation in females
Study here.
Did you catch that brain area?
Men relied on the prefrontal cortex (part of our anxiety circuit that offsets fear response) while women relied more heavily on "limbic areas" where the amygdala resides.
That's our fear and threat detection brain area!
This doesn't mean it dictates our response...just a specific bent on the stress response.
The brain is use it or lose it.
If we're using the amygdala more on average, it tends to gain volume and function.
We'll discuss below how women can strengthen the prefrontal cortex to offset this "bias".
It's also been shown to have a documented effect on anxiety and depression for both genders! (that's a bonus).
Interestingly, downstream, men tend to respond more strongly to stress in their bodies:
Relatively higher secretion of ACTH with comparable total cortisol levels under basal conditions has been observed in men
https://www.ncbi.nlm.nih.gov/pubmed/8392084/
ACTH is adrenaline essentially.
This affects how they attempt to resolve stress:
While men are less likely to verbally report distress and anxiety, they may tend to experience anxiety at a more physiological level and engage in more action-oriented stress coping
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5123837/
Does this sound familiar?
My husband always wants to solve an issue when stress arises but I'm really just looking to express and talk it out.
I have to constantly remind him, "I don't want to solve it...I just need to get this out".
In fact, researcher found a gene SRY which drives the fight or flight response in the body. Women don't have this gene (it's on the sex chromosome that only men have) and there's a theory that women...wait for it... process response to stress elsewhere (involving estrogen system).
Since women don't have the SRY gene, their responses to stress are regulated by other genes and other physiological changes involving estrogen hormones and, as previously mentioned, oxytocin and endorphins.
As they stated, you can put two male chimps (strangers) in a cage and they'll try to kill each other. With two females, they will exchange grooming to bring down the awkwardness.
Let's now jump to immune systems.
Interestingly, autoimmune disease hit women at a much higher rate than men.
Check out our massive our review of CBD and autoimmune here.
In fact, the ratio is pretty comparable to what we see with anxiety!
Hmmmm.
Look...immune response is the new future of medicine right now.
Check out CBD, neuroinflammation, and anxiety to see just how powerful this effect is for anxiety.
Interestingly, there's a connection on people who took SSRI's and autoimmune activity:
A particularly important observation was that, for those with PTSD who were being treated with an SSRI (a type of antidepressant), the increased rate of autoimmune disease was less dramatic.
https://www.health.harvard.edu/blog/autoimmune-disease-and-stress-is-there-a-link-2018071114230
This is a clue (serotonin) we can use below.
Both genders experience inflammation, but are there differences in the brain's ability to repair and rebuild?
Notice this little nugget here:
Women have an increased lifetime risk of stroke compared to men, largely due to a steep increase in stroke incidence in older postmenopausal women, yet most basic science studies continue to only evaluate young male animals.
https://www.ncbi.nlm.nih.gov/pubmed/27870410
"Postmenopausal" = steep increase.
Let's introduce BDNF, a powerful "fertilizer" in the brain.
Studies are pointing to gender differences in BDNF:
In particular, BDNF content in some brain parts and the tendency of developing BDNF-deficient-related diseases like depression is higher in female animals.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5271179/
Look...BDNF is written all over the research for anxiety.
It's a primary support system for serotonin function which is how SSRIs (Effexor, Lexapro, etc) work till they build tolerance!
BDNF repairs serotonin neurons and serotonin spurs BDNF activity!
Check our review for CBD, BDNF, and anxiety to see just how important it is.
More important to our discussion on perimenopause anxiety is the effect of hormones:
Indeed, the cross-talk between BDNF and sex steroids has been detected for decades and some sex steroids like estrogen have a positive regulatory effect on BDNF expression and signaling.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5271179/
Guess what drops through the floor during perimenopause?
Estrogen!
Actually, it tends to spike and drop during the throes of perimenopause but eventually...it's down from there.
Finally, researchers found a direct pathway different between the genders that has an immediate effect on the anxiety circuit.
Interestingly, it involves the endocannabinoid system!
Essentially, the difference affected how GABA and Glutamate function in the brain.
GABA is the key lever for benzos (see CBD versus benzos for GABA and anxiety).
Specifically, Woolley and her research team found that in female brains the drug URB-597 increased the inhibitory effect of a key endocannabinoid in the brain, called anandamide, causing a decrease in the release of neurotransmitters.
https://www.sciencedaily.com/releases/2015/08/150812135651.htm
Ohh….this is interesting. Stick with us.
That URB-597 blocks FAAH. FAAH eats up Anandamide.
Anandamide is our so-called "Bliss" molecule.
To see just how powerful they both are for anxiety, check out our article on the woman who can't feel pain or anxiety (or depression) because she lacks FAAH.
What about men?
In male brains, the drug had no effect. (The difference is not related to circulating reproductive hormones.)
Put a checkmark next to anandamide and FAAH for later with CBD.
So those are a few gender differences out of many.
The research paints this narrative:
- Women respond to stress differently (the damage)
- The repair/replenish pathways respond differently (the repair)
- Hormone and endocannabinoid systems respond differently (the balancing of both)
Let's move on to the critical period of perimenopause.
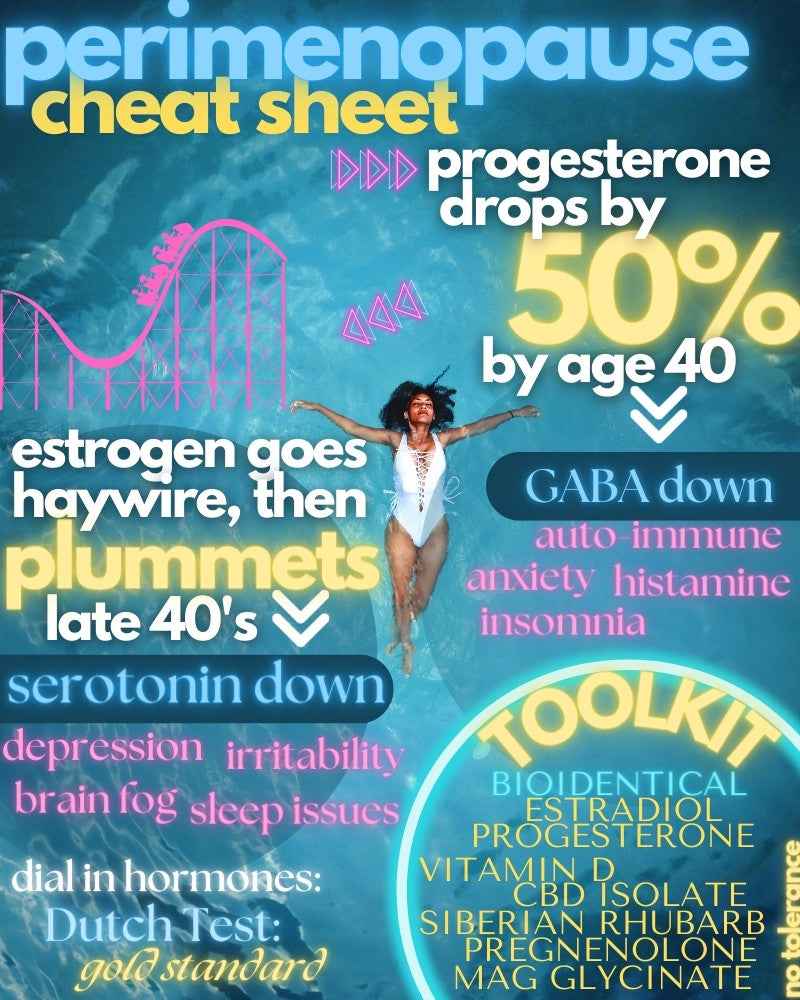
Why does perimenopause cause anxiety
First and foremost, perimenopause is a hormonal story.
It reflects a significant drop in key steroidal or sex hormones.
People (including most of our medical profession) tend to think of these hormones only in terms of reproduction.
Goodness, that couldn't be further from the truth.
You have estrogen receptors on every critical system in your body.
Muscle. Heart. Bone. and yes...Brain.
Interestingly, women with high baseline anxiety before perimenopause continued to experience it but what about women with low anxiety states prior?:
Women with low anxiety at baseline were more likely to report high anxiety symptoms when early or late perimenopausal or postmenopausal compared to when they were premenopausal (odds ratios ranged from 1.56 to 1.61), independent of multiple risk factors, including upsetting life events, financial strain, fair/poor perceived health, and VMS.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641149/
After all our research and everything I've been through, the "early or late" piece makes sense.
It's the time of most change.
Your body is used to a rhythm that occurs about the same each month for decades and then it changes.
That's stressful in itself.
It's also why we see anxiety tied to other hormonal changes such as during the monthly cycle, pregnancy, delivery, and the like.
If we want a snapshot of changing hormones, we can look at the monthly cycle.
Here, we have to look at estrogen and progesterone.
These are the so-called sex or steroidal hormones.
Men have them but not to the extent and complexity that women have them.
We think of them in terms of reproduction but they're intimately tied into almost every system in your body and brain.
Let's focus on the brain:
Sex steroids affect mood and anxiety by mediating changes in neurotransmitter systems in a diverse array of brain regions
Across our articles, we've looked at serotonin (CBD versus SSRI for serotonin) and GABA (CBD versus Benzos for GABA) extensively.
Are there even hormone receptors in these pathways?
CNS activities of noradrenaline, dopamine, serotonin (5-HT), and g-aminobutyric acid (GABA), which are implicated in the pathophysiology of anxiety, are all affected by female sex steroids.
You can pick any neurotransmitter and any sex hormone and find a choreographed dance of interactions between the two.
For example, let's look at estrogen and serotonin (the target of SSRI's):
Overall, estrogens exert an agonistic effect on both 5-HT and noradrenaline activities by increasing their synthesis and release, inhibiting their reuptake, and slowing their degradation
5-HT is serotonin! It's intimately tied with BDNF and brain repair and replenishment.
Don't get us started on estradiol (one of the three flavors of estrogen) and the other lever for anxiety.
We did a giant review on estrogen replacement or estrogen and mental health.
Then there's GABA!
Gaba is the "brake" in the brain and it's intimately tied to anxiety, sleep, and a host of other issues resulting from perimenopause.
In fact, GABA is the direct target of benzos, the most common medication of perimenopause anxiety (with huge drawbacks - see CBD versus benzos).
Remember how anxiety can be tied to hormonal shifts such as the monthly cycle or the big cycle of perimenopause?
Fluctuations in the sex-steroid environment during reproductive cycles are highly associated with changes in GABA receptor subunit composition in the brain
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2787920/
you think???
We're finally getting newer research teasing out the relationship:
Our data indicate that the estrogen may increase the number of GABA binding sites by direct interaction with the GABA receptor gene or genes involved in the metabolism of the GABA receptor.
https://www.fertstert.org/article/S0015-0282(18)30677-0/pdf
Estrogen is a major string-puller for GABA's action in the nervous system as well.
And it's spiking and dropping during perimenopause!
Again, the endocannabinoid system appears to mediate these effects:
We found recently that 17β-estradiol (E2) acutely suppresses GABAergic inhibition in the hippocampus of female rats through a sex-specific estrogen receptor α (ERα), mGluR, and endocannabinoid-dependent mechanism
https://www.jneurosci.org/content/35/32/11252
We'll get into that below.
Then there's estrogen's effect on BDNF, our brain's "fertilizer" and key to ½ of the anxiety circuit (repair).
In an interesting study, researchers could supplement estradiol and improve performance with mice.
This improvement disappeared in mice where BDNF pathway was reduced:
In another study using BDNF heterozygous (+/−) mice, it is reported that estradiol replacement improved the performance on Y-maze and novel-object recognition test in ovariectomized wild-type but not in ovariectomized BDNF+/− mice (
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5271179/
Basically, when they blocked BDNF activity, replacing estradiol no longer had its positive effect.
BDNF is written all over the anxiety circuit (see CBD and BDNF for anxiety).
We could go on and on. Estradiol's important!
So much so that we wrote a huge review of Estradiol for perimenopause here.
Then there's progesterone.
We can look to the monthly cycle to see the importance of progesterone on the anxiety circuit.
Many studies find an increase in anxiety premenstrually.
In fact:
Similarly, 79% of women with PD reported that they experienced an exacerbation of anxiety premenstrually
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3176921/
This is the time when both estradiol and progesterone are dropping.
Looking at BDNF, the brain's "fertilizer" for repair, progesterone directly figures into this:
Progesterone, another important sex steroid produced mainly in the ovary, can also increase the production of BDNF in the cortex explant and glial cells
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5271179/
Progesterone is known to be neuroprotective and BDNF may be the key:
Based on the result of these studies, it has been suggested that progesterone-mediated neuroprotection is BDNF-dependent.
What's really interesting is how progesterone works:
Progesterone acts as an allosteric modulator of GABA, with its anxiolytic effects attributed to the metabolite, allopregnanolone, on the GABA-benzodiazepine receptor complex (GBRC)
Let's break that down because it's important!
Allosteric modulator of GABA means that is works like a reverse messaging system.
For example, benzos go only one way….boost GABA levels.
Allosteric means that the receiving neuron sends a message back, saying "Hey, we're good here or send more GABA over".
It's a check and balance system.
Guess what else works that way…
CBD! That's only the start of that result.
Anxiolytic means anti-anxiety because...any opportunity to make things more complicated.
Finally, allopregnanolone!
Don't get us started on this.
Allopregnanoloneenolone is one of the chemicals that progesterone breaks down in to.
It's the basis for the brand new post-partum depression (ding ding ding) medication that's $25K month.
You can get pregnenolone (full review on pregnenolone here) for $10 and it breaks down into progesterone AND allopregnanolone!
It also happens to be an endocannabinoid (one of three hats it wears).
The point is this...progesterone and its cousins have powerful effects on the anxiety circuit.
Look, general anxiety state (see CBD and general anxiety disorder), as well as socio-psychological stress (differences in income, roles, etc), come into play even between women themselves.
That being said, hormones are the key lever in perimenopause and the bulk of effects likely reside there for anxiety.
Does perimenopause anxiety go away
This is a common question and one usually born out of a state of anxiety!
I've been there, asking my husband many times…
"This is going to stop, right???"
That was back in the dark days before getting relief from bio-identical hormones, CBD, and a range of supplements and lifestyle changes.
The hormones had the biggest impact by far.
It's important to understand the two phases.
Perimenopause is about change. This much change is stress in the body.
If a body is already struggling with stress response or repair, this can be rough.
Eventually, the hormones drop to very low amounts and stay relatively stable.
That's another set of problems since hormones are intimately tied to every system in your body.
As for perimenopause, that "flux" drives the issues.
Most women don't realize that they probably started it back in their early 40's when the hormones (mainly progesterone) start to drop.
It generally reaches a fevered pitch late 40s and can run a few years.
Technically, you're out of perimenopause and into menopause 12 months after having your last period.
Keep in mind that it goes out in fits and starts.
The ovaries can go out one at a time and/or suddenly release hormone in spurts.
Those are always fun :)
More importantly, you can have progesterone and estrogen dialed in at the beginning and your levels continue to drop.
The hormone flux aspect of perimenopause anxiety will stop.
The lack of total hormones afterward is another story.
We have deep dives on the hormones here:
Progesterone for anxietyEstrogen for anxiety
The goal during perimenopause is to address the balancing system in the body...the endocannabinoid system and optimize core pathways.
We'll look at that below.
First, a quick jaunt through the standard medical approach...which almost did me in.
The standard medical approach for anxiety during perimenopause
My experience is pretty common.
First, if you walk into a doctor's office in your late 40's with sudden anxiety or panic attacks, the course will probably run this way.
A first hit of benzos (Ativan, Valium, or Xanax).
All short term fixes and highly addictive.
What do they do?
They spike GABA levels!
Check out CBD versus Benzos for anxiety
They also increase dopamine which is why they're so addictive.
Plus your brain (already in flux) then starts to reduce natural levels of GABA as a knee jerk reaction.
Classic normalization effect (need more and more for the same effect).
It was pretty rough coming off of these as I described in the CBD to wean off benzos article.
Again, the benzos come with a warning that they're only intended to be short term...weeks at most.
They do nothing for the mechanism of anxiety...just wrap in a dull, fuzzy blanket temporarily.
Next up (if not the first option), they will offer SSRIs like Lexapro, Effexor, or Zoloft.
What do these do?
They boost serotonin availability (we saw this quite a bit up above).
See CBD versus SSRI for serotonin and anxiety.
They don't have a classic addiction piece but good luck getting off of them.
They come with a warning not to drop them quickly!
The side effects list is long, varying, and strange.
In fact, the doctor will probably give you benzos for the first 2-3 weeks because SSRI's actually can INCREASE anxiety and depression at the start.
Check out CBD and corticotrophin-releasing factor for the reason why.
Also, I went through coming off of Lexapro with CBD to wean off SSRIs for anxiety.
Research is basically saying that SSRI's true effect is boosting brain repair (serotonin and BDNF are intimately related). till tolerance ekicks in
We go through the relationship at our How SSRIs really work page.
SSRIs also normalize (effect goes away) so you have to switch among them generally.
To see the importance of perimenopause and serotonin:
In particular, estrogens increase serotonergic activity by regulating 5HT metabolism and 5HT receptor expression, as well as modulating the spontaneous firing of the serotonergic neurons in the raphe nuclei
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6335777/
Let's look at what your doctor probably won't do (for a woman in her 40's who suddenly losing her $%&!).
He/she probably won't run a Dutch test or something similar to see where your hormones are.
They probably won't look at pregnenolone, bio-identical hormones, Siberian Rhubarb, and core nutrient levels (D, B's, inflammatory markers, etc).
We have a complete review of Estradiol here and Siberian Rhubarb.
You're likely reading this after being through that rinse-repeat cycle.
Good...let's now see what we can do about it!
One-stop before CBD and other tools for perimenopause anxiety.
The endocannabinoid system and perimenopause anxiety
We've mentioned this system a few times up above but let's get into it!
It may be the linchpin for perimenopause anxiety.
Why?
Every woman has this system.
In fact, all animals have one!
It's generally tasked with balancing (homeostasis) other key systems:
- Nervous system - neurotransmitters including GABA, Serotonin, BDNF and others
- Immune system - inflammatory agents such as microglia, cytokines, and the gut
- Endocrine system - hormones like estrogen, progesterone, and others!
Did you catch that last one!
That's the crux of perimenopause anxiety and flux.
Significant drops in estradiol and progesterone (pregnenolone, the mother of all sex hormones has been dropping for decades!).
You're about to be light years ahead of every woman you know (unless they've read this!).
Simply put, this system is tasked with responding to stress or change and re-calibrating the system.
Um...change? Stress?
Can we just say perimenopause...the greatest change to a woman's body, equal to puberty (and that was loads of fun!).
The difference is that puberty occurred when all our systems were functioning at full speed.
- Repair (jacked up to the gills) which is why we can learn so easily then - BDNF.
- Mitochondria and energy - mitochondria accumulate errors over time and it may be the Jenga piece that brings everything down in terms of aging
Fast forward 3 decades!
Now try to go through that level of change.
And is anxiety really that surprising?
These are early days still (thanks to medical research...it's just half the population) but try to unravel the clues.
First, a study found that positive hormone replacement therapy benefits could be extended with a corresponding boost to CB1 receptors (main endocannabinoid receptor in the nervous system):
The present study demonstrates that an HT time window in mice can be prolonged by cotreatment with a CB1 agonist, implying a potential strategy for HT in long-term menopausal women.
https://www.jci.org/articles/view/123689
HT is hormone replacement therapy. There was an issue with women who started hormone replacement later in the process missing out on protective benefits.
The endocannabinoid system seems to aid in extending this window!
That's a 2019 study...like we said...research is late to the party.
Let's get into the most exciting connection between the drop in hormones and this system.
Estradiol and FAAH.
First, an introduction to the chemicals in your body that literally make you feel pain and anxiety (and depression).
That's a bold statement but bear with us.
Anandamide is our 2nd most prominent endocannabinoid (naturally occurring) in the brain.
It's called our "bliss" molecule and named after the Hindu goddess of bliss, Anand.
So far so good...bliss.
FAAH is an enzyme that breaks down anandamide.
There's a genetic variant of FAAH (makes way too little) where people are unable to feel pain, anxiety, or depression.
Check out our review on the woman who is unable to feel these feelings.
Increased FAAH and the resulting decreased Anandamide are all over anxiety!
See CBD and anxiety here.
So...what does this have to do with perimenopause anxiety?
One experiment found that estradiol directly modulates anandamide levels.
In fact, they found that estradiol dampens the fear response (avoid) center of the hippocampus through anandamide:
E2 acts through the α form of the estrogen receptor to stimulate the postsynaptic mGluR1-dependent mobilization of the endocannabinoid anandamide,
https://www.sciencedirect.com/science/article/pii/S0896627312003753
More interestingly for perimenopause:
Remarkably, this effect of E2 is sex-specific, occurring in females but not in males.
E2 is estradiol.
Okay...so estradiol is dropping rapidly during perimenopause.
Now, we're going to look at our favorite study.
Basically, they look at mice with their ovaries removed (a more sudden perimenopause if you will).
When they supplemented estradiol, it resulted in anti-anxiety and anti-depression effects to counter the results of losing their ovaries.
Guess what happens when they block endocannabinoid function (CB1) to this effect of estradiol:
Interestingly, however, anxiolytic- and antidepressant-like effects produced by estradiol administration are attenuated by CB1R blockade [112], whereas estradiol administration increases AEA levels
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4169112/
AEA is anandamide.
Look, this is really important so let's go back through it and simplify.
- Remove ovaries (and estrogen) and anxiety and depression resulted
- Supplement with estrogen and anxiety and depression subsided
- Block endocannabinoid system and the supplementation of estrogen didn't work!
Goodness.
Many studies have looked at FAAH and anxiety in mice lacking estrogen:
Despite these differences, FAAH inhibitors retain anxiolytic- and antidepressant-like effects in ovariectomized female rats
Basically...block FAAH (which increases anandamide) and anti-anxiety and anti-depression effects occur.
We were so fascinated that we did giant reviews on boosting endocannabinoids and endocannabinoid defiency.
Could it be that the endocannabinoid system is the difference between men and women for anxiety, panic attacks, and depression?
Could it also be the linchpin for perimenopause anxiety?
Researchers went on to say:
These observations suggest that FAAH–AEA signaling may be one important mechanism linking gonadal hormone status and account, at least in part, for sex differences in anxiety.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4169112/
Another study looked at estradiol and emotional response to stress.
Guess where the intersection was?
Estrogen recruits the endocannabinoid system to modulate emotionality.
https://www.ncbi.nlm.nih.gov/pubmed/17391861
There's lots of interesting research on the fear response, fear extinction, and a range of pathways that lie at the intersection of estrogen and endocannabinoids.
Let's jump to CBD.
Can CBD help with perimenopause anxiety
We've covered CBD's benefits for anxiety here.
There is a great deal of research on CBD and the many different facets of this pathway.
Let's focus on those tied to perimenopause, and most importantly, its loss of hormones.
We look at some key aspects tied to the loss estradiol and progesterone:
- Reduction in the serotonin pathway (target of SSRI's)
- Reduction in BDNF (brain fertilizer)
- Estradiol boosting of GABA (target of benzos)
- Stress response difference in women (Amygdala focus)
- FAAH and Anandamide levels
Let's focus down on those.
We'll start with the repair side (serotonin, BDNF).
What does CBD do there?
Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain.
https://www.ncbi.nlm.nih.gov/pubmed/30157131
The keyword there is "modulate". Allodynia just means a lowered pain threshold.
It doesn't jack it up like SSRI's which is where all the side effects come from.
Let's dig a little deeper into this effect.
We'll bring back in what estradiol did from above:
In particular, estrogens increase serotonergic activity by regulating 5HT metabolism and 5HT receptor expression, as well as modulating the spontaneous firing of the serotonergic neurons in the raphe nuclei.
Okay, estrogen "modulates" serotonin activity in the raphe nuclei.
And CBD?
Seven days of treatment with CBD reduced mechanical allodynia, decreased anxiety-like behavior, and normalized 5-HT activity
Where?
5-HT neurons in the dorsal raphe nucleus
Goodness. 5-HT is the serotonin pathway.
Did you catch that word, "normalized"?
This is the beauty of CBD and really the endocannabinoid system in general...it's about balance.
Allodynia is pain threshold.
By the way, joint pain is a major symptom of perimenopause.
We can see how dropping estradiol reduces serotonin function and this experiment explained how reduced pain threshold is the result!
That's another article here.
Check out CBD versus SSRI for serotonin!
Serotonin is highly integrated with BDNF, our brain's fertilizer.
BDNF is all over anxiety (maybe even more important than serotonin as a root cause).
Can CBD affect the BDNF function?
Cannabidiol Induces Rapid and Sustained Antidepressant-Like Effects Through Increased BDNF Signaling and Synaptogenesis in the Prefrontal Cortex.
https://www.ncbi.nlm.nih.gov/pubmed/29869197
From all our studies, the thing that comes across is that anxiety and depression are partially the result of a brain not being able to repair itself from stress, infection, our immune system and inflammation.
BDNF and serotonin are key to this neurogenesis effect.
Now to the damaging side.
We've written extensively on CBD and stress, inflammation, and neuroinflammation.
You can get access to all of these elements and more at our CBD and the mechanisms of anxiety.
Some unique takeaways for perimenopause.
There's an interesting study that shows that women's stress response works differently than men's is one specific pathway.
Basically, when the chemical trigger for stress (corticotropin-releasing hormone) is released, men's stress response will use oxytocin (the nurturing chemical of all things) to negate its effect:
production of CRHBP blocks the CRH-induced potentiation of postsynaptic layer 2/3 pyramidal cell activity of male, but not female, mice, thus producing an anxiolytic effect.
https://www.ncbi.nlm.nih.gov/pubmed/27641503
That's all technical but the net-net is this…
Can we reduce the effect of CRH and boost oxytocin during perimenopause with CBD?
Yes!
New studies can actually look at gene expression on this front:
Interestingly, cannabidiol at low (5 mg/kg) and intermediate doses (15 mg/kg) successfully blocked the effects induced by acute stress on corticotropin-releasing factor, pro-opiomelanocortin, and glucocorticoid receptor gene expression.
https://journals.sagepub.com/doi/abs/10.1177/0269881118805495?journalCode=jopa
Check out CBD and Corticotropin-Releasing Factor (CRF) for more info.
As for oxytocin, new studies on autism (a lack of oxytocin function) are showing that the endocannabinoid system is all over its function:
The results indicate that anandamide-mediated signaling at CB1 receptors, driven by oxytocin, controls social reward.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4653148/
That's a great segue.
We saw from above that FAAH and anandamide are probably the biggest levers we can push for perimenopause anxiety.
This may be CBD's crown jewel effect of the different pathways affected.
Right to the point:
CBD increases anandamide levels by inhibiting its transporter-mediated reuptake and degradation by FAAH
If that wasn't enough:
CBD also binds to the fatty acid-binding proteins that transport anandamide intracellularly to FAAH for its degradation, which may play a role in the inhibition of anandamide metabolism by CBD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6486906/
And why does this matter for perimenopause anxiety?
Elevating anandamide levels systemically or centrally via the pharmacological inhibition of FAAH is well known to produce anxiolysis, particularly under more aversive conditions
Anxiolysis is just a fancy way to say anti-anxiety.
Also, CBD and GABA for anxiety since it's THE lever for relief right now (as opposed to long term).
Let's look at some other helpful things I've found along the way.
Other supplements for perimenopause anxiety
Perimenopause can be a maelstrom.
It requires that we optimize our nutrients and resiliency.
These are some important tools I've used and researched to navigate this period of time:
- Bio-identical estradiol and progesterone
- Pregnenolone - the mother of all hormones (see full review here) -
- Exercise (boosts BDNF and reduces stress response)
- Mindful meditation (see CBD and mindful meditation for neurogenesis)
- Yoga - same effect as mindful meditation
- Methylated B vitamins (if you're one of the 40% that has MTHR or MTHFR gene variants)
- Magnesium (essential!!! Glycinate or Theorate)
- Vitamin D - almost everyone is deficient...I'm trying to get mine to 65 and 5000 is slowly moving the needle
- NAC - boosts glutathione, our natural anti-oxidant - see CBD and glutathione
- Probiotic - gut health IS health - see CBD and probiotics for ties to anxiety
- NAD - energy production
- Zinc and mineral support
- Vagal nerve stimulation via the ear - very cool, new research see here.
Most of these things "upregulate" key genetic pathways that will be sorely lacking under the stress of perimenopause.
Just a head's up...the go-to self-medication appears to be alcohol for women in perimenopause.
Alcohol boosts GABA!
Go figure.
The problem is that it's also broken down into a poison called acetaldehyde.
That's a load on your liver and glutathione system.
We get it...some women towards the end of the day are literally shaking during perimenopause.
Just see if you can get your GABA a different way and CBD can help with detox (see CBD for oxidative stress) and even help protect the liver and brain:
Transdermal delivery of cannabidiol attenuates binge alcohol-induced neurodegeneration in a rodent model of an alcohol use disorder.
https://www.ncbi.nlm.nih.gov/pubmed/24012796
If you do drink alcohol, at least use CBD to offset some of the negative effects.
We'll write an extensive review on that whole situation because it's so prevalent.
Not judging, just looking out for you since so many of my friends ARE you.
Back to CBD...how much to take?
How much CBD to take for perimenopause anxiety
We have research on anxiety itself and all the pathways are the same albeit, downstream from drops in hormones.
Neurogenesis, the key to long term repair for anxiety circuits is shown to peak at 300 mg of CBD.
More info here at our review of how many mg's of CBD for anxiety.
Most people start around 25-40 mg to test their response.
Sleep help is shown at about 160 mg.
Beyond that, it depends on your system and your state.
If you're in a really bad way like when I started, studies used 600 mg for more serious issues.
The public speaking anxiety study for CBD was at that amount.
There's a short term and long term aspect of this.
Test and adjust. That's the tried and true approach.
One note...CBD can interfere with metabolism of other medications so check with your doctor.
Finally, some important words on the kind of CBD.
What's the best CBD for perimenopause anxiety
This drives us crazy.
Everyone out there, even the legitimate big brands, are pushing full-spectrum CBD.
Learn about CBD isolate versus full spectrum for anxiety here.
As a result, many women during perimenopause have bad reactions to their CBD.
That's a histamine response!
40-60% of the population has histamine issues.
Guess what...your allergic or histamine response gets worse during perimenopause! (Thanks for leaving, progesterone).
Women are already hit harder on this front.
All that plant material in full-spectrum CBD is going the wrong direction.
That's why we only deal with CBD isolate.
I personally tried 3-4 of the biggest brands at the beginning and had an allergic response.
If you're like me, you'll notice during perimenopause that you're much more sensitive to chemicals, foods, and the like.
It's not just us...research backs it up:
Around 30–40% of women who have asthma experienced worsening of their symptoms during the perimenstrual phase, the so-called perimenstrual asthma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377947/
Plus...the little factor that all the research is on CBD isolate.
Like we said in the beginning, we're all about the research and that's what we built IndigoNaturals on.
This glimpse into perimenopause is just the beginning. 'Dre's Story' offers our complete, research-rich journey into hormones, tools to feel better, and safety. The full Perimenopause Toolkit with new additions can be found Here. Please review so other can learn. Feeling better starts with understanding what is happening.
Get specific links for CBD and Perimenopause symptoms and questions here.
Related Research:
Why some women get hit so hard with perimenopause
The CBD and Anxiety Ridiculous Guide
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.