Why Perimenopause is Different from Menopause - The Complete Story

I had no idea what I was in for.
It looks like many women don't!
Why don't we ever learn about this in our early 40's so we can be ready and manage it successfully.
After the entire, crazy experience, I now see that this transition is treated like a dirty secret...a taboo that women shouldn't broach.
Look...I could have avoided so much suffering had someone given me a head's up.
Apparently, I'm not alone.
Roughly 25% of women have severe perimenopause transitions. Debilitating.
In fact, if you do all the research we have, its hard to even get information on perimenopause versus menopause...but…
They are SO different from each other.
We're going to get into all of it including the questions I had and the ones you may face (via running into a wall!).
I received so much bad advice from many doctors when this first started and I would have loved a comprehensive look at perimenopause as a transition to menopause.
That story is here but we're a few years out now so let's get to work.
We'll cover these topics:
- What is the difference between perimenopause and menopause
- What age does perimenopause and menopause start
- How long do perimenopause and menopause last (hopefully long for the latter)
- How do I know when I'm in perimenopause or menopause
- Are the symptoms worse in perimenopause or menopause
- How long do perimenopause and menopause last (hopefully long for the latter)
- How do I know when I'm in perimenopause or menopause
- Why do some women get hit so hard with perimenopause?
- How do I get through perimenopause and menopause successfully (translated...with sanity intact)
Let's jump into it.
What is the difference between perimenopause and menopause
There's a great deal of confusion on this part and if you're like me, you have no idea what to look for til you hit a brick wall.
Perimenopause is very different from menopause!
On the surface, perimenopause is the transition to menopause.
That's like saying puberty is the transition to reproductive years.
Yes, it's true but clearly puberty can be a period of intense flux.
Same thing goes for perimenopause.
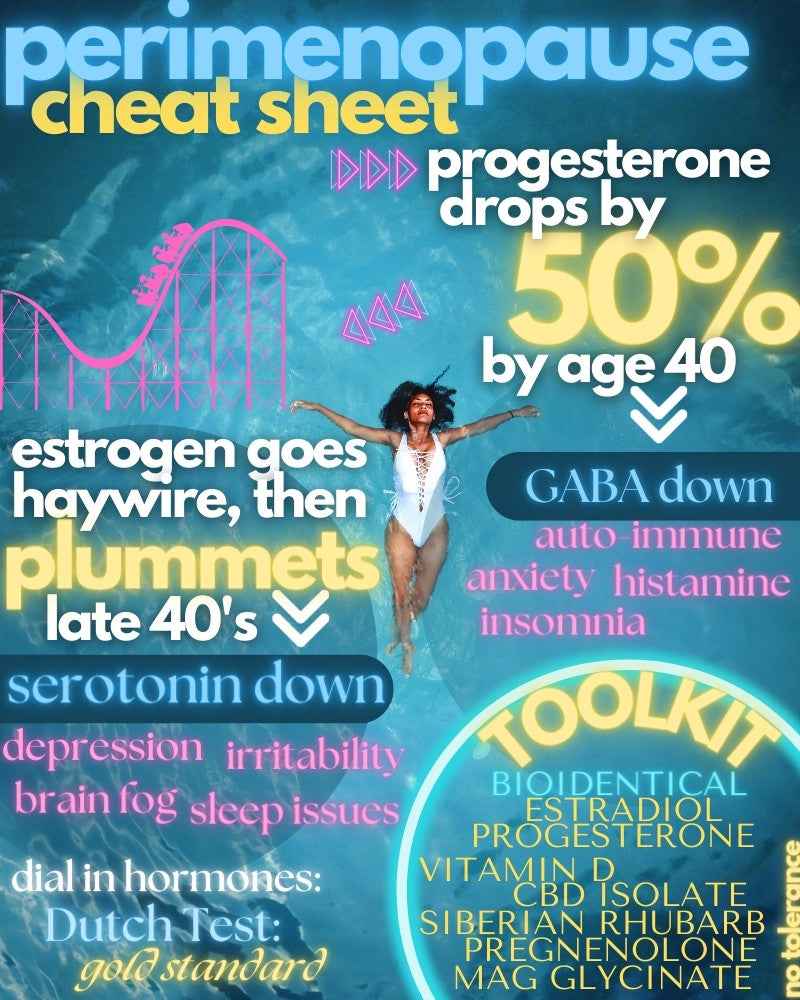
Essentially, the main reproductive hormones are winding down during perimenopause.
We're talking about progesterone and estradiol (our main estrogen - E2) primarily.
Here's where most websites and doctors get it wrong.
The progesterone drops off fairly smoothly and starts much earlier (we'll get into timetables later) but estradiol may not go quietly into the night!
As I learned the hard way, it's the "flux" of estradiol that can really send women to the breaking point.
I'm not alone.
It's estimated that 25% of women will have debilitating perimenopausal symptoms.
Dre's story is here but I can definitely relate.
So...what's going on there?
First, understand that estradiol is incredibly important to our bodies and brains.
Just check out the review on estradiol for perimenopause or estrogen and mental health.
Bone. Brain. Heart. Almost every cell in your body has an estrogen receptor (comes in two flavors: alpha and beta).
For one simple example, estradiol controls both the production and elimination of serotonin, our workhorse neurotransmitter in the brain and gut.
That speaks to the go-to prescription most women will get for a bad perimenopause...SSRI's such as Lexapro or Zoloft.
Lexapro nearly ended me but that's another article.
See CBD versus SSRI's for serotonin or CBD for perimenopause depression.
The effect during perimenopause?:
This relationship between estradiol and serotonin is prominently featured in perimenopause, when estradiol levels eventually plummet, leaving serotonin down in the dumps as well.
https://www.zrtlab.com/blog/archive/impact-hormones-serotonin-depression
That's just one example...estradiol is a powerful force OUTSIDE of reproduction!
The issue is that most of the medical world sees perimenopause in the same light of menopause when hormones are low and more stable.
That couldn't be further from the truth:
Evidence shows that with disturbed brain-ovary feedbacks, E2 levels average 26% higher and soar erratically – some women describe feeling pregnant
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987489/
The spikes in estradiol (and erratic changes in body or brain) is what was so scary if you don't know this little fact.
For example...if perimenopause is just a gradual lowering of hormones, you shouldn't see swings from one day (hour) to the next!
That's what men "enjoy" with testosterone's slow decline.
This is frightening (think of hormones as a lens through which you emotionally view the world) until you understand what's really going on.
Let's go there!
So what happens as it starts to drop during perimenopause?
The body panics.
Actually, the estradiol overseer called FSH.
FSH, short for follicle-stimulating hormone is intimately involved in the monthly cycle dance.
First, FSH drives estradiol production:
FSH stimulates the follicles — the fluid-filled sacs in the ovaries that contain the eggs — to produce estrogen.
https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
Conversely…rising estradiol should block FSH.
A seesaw if you will.
The problem during perimenopause is that it can become a roller coaster.
FSH tries to produce...one….last…..egg (for dramatic effects - the cheesy death scene in a movie if you will).
It juices the levels of estradiol.
This can actually cause spikes in estradiol during perimenopause which is where most doctors go wrong.
They think of estradiol being on a slow decline into a graceful menopause.
They must be men!
A better chart can be found here:
https://www.zrtlab.com/blog/archive/mood-menopause-perimenopause/
Think of perimenopause as an extended PMS...a 30 day cycle stretched out.
This leads to a cat and mouse game between FSH and estradiol which can literally be excruciating.
Just check out CBD and perimenopause anxiety since anxiety is a key symptom of this yo-yo effect.
Towards the end of perimenopause, estradiol production from the ovaries drops to nothing.
There's nothing left to juice from FSH and that spiking of estradiol drops.
Production of estradiol (since it's so essential) then moves to the adrenals which leads to often diagnosed "adrenal fatique" which is really just a lack of estrogen!
In the meantime, estradiol can jump to twice the normal levels compared to earlier in life.
The dance is offbeat:
In these cycles, the secondary, luteal rise of estrogen is maintained and even exaggerated, and leads to a subsequent cycle in which progesterone production is deficient. The investigators attributed this pattern to sustained FSH elevation, which ‘drove’ estrogen production in the subsequent cycle
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3197715/
Again, check out the estradiol and perimenopause review to see how powerful the effect can be.
If you're reading this, you probably already know!
So...when does all this start?
What age does perimenopause and menopause start
We really have to look at this in two parts and note that there's a tremendous amount of variability.
Over at the perimenopause Reddit boards, you'll see women who are shocked to start the process in their late 30's and early 40's!!
This is really early but becoming more common these days.
The first leg is progesterone and that starts to drop for most women late 30's and early 40's.
By the time you reach perimenopause, it's pretty low and mine was almost undetectable.
Interestingly, you may run out of progesterone even before losing your period.
They are called anovulatory cycles.
If there's no egg release, there's no resulting progesterone.
Progesterone loss tends to be more gradual but not it's opposing force, estradiol.
Most of the perimenopause craziness is from estradiol fluctuations and eventual drop.
The general age for this is from about 48-52 as a range.
Again, it can come much earlier for some women.
Officially, it kicks off when you start to miss periods but the process can show earlier with symptoms:
- Irregular periods
- Incontinence
- Mood changes such as anxiety, depression, panic attacks, irritability, etc
- Sleep disruption
- Hot flashes
- Ovarian cysts
I was "fortunate"...I had all of them!
Once it starts, how long does this crazy ride last?
How long do perimenopause and menopause last (hopefully long for the latter)
Technically, the medical world looks at perimenopause as the time prior to 12 months without a period.
That's great and all but the actual period of transition can be a few years.
For example, I didn't start to lose my period until May of 2019 but the real roller coaster started in 2017.
Some signs (irregular periods, panic response, etc) started a few years prior to that.
The cat and mouse game between FSH and estradiol depends on when your estradiol starts to wane which is a function of your available follicle count.
On average, it's looking like a 2-3 year window for the most severe part of perimenopause loosely ending after 12 months of no period.
There's just nothing left for the FSH to squeeze out of the ovaries in terms of estradiol.
You can't spike what you don't have!
Menopause then follows with reduced levels of estradiol and progesterone, raised FSH, and slow progression to very low hormones.
This has its own issues since estradiol and progesterone are so important to many other facets of our health - both body and brain.
Menopause is the final stage so that continues.
Interestingly, where men's testosterone eventually levels out and stops dropping, women's estradiol continues down to almost nothing.
That's not good for bone, brain, heart, and more.
For me, bio-identical hormone supplementation was the difference between functioning versus checking out. Quite literally.
More on that here.
How do I know when I'm in perimenopause or menopause
Unless you have a great doctor who starts running your baseline hormone panels in the 30's, you'll probably get the notice via symptoms.
Again...why OBGyn's don't establish each woman's early (20's) baseline hormone panel (estradiol, progesterone, and testosterone, at least) is beyond comprehension.
They really ONLY see them as means to reproduction.
That will change but in the meantime, demand your hormone panel annually.
If you're reading this, that time has probably passed but pass it on to younger siblings, daughters, and friends.
We need to look out for each other!
So...how do we know?
For perimenopause, the early telltale signs are:
- Irregular or changes in cycle and/or period (this may occur years before 12-month loss of period)
- Changes in weight, cholesterol (see review on pregnenolone), fatigue, or sleep
- Changes in mood including anxiety, depression, panic response, irritability
- Incontinence, UTI's, changes in immune response
- Histamine or allergy increases (big signal to progesterone depletion)
There's a great review of what to look for in terms of symptoms:
- New-onset heavy and/or longer flow
- Shorter menstrual cycles (≤ 25 days)
- New sore, swollen or lumpy breasts
- New mid-sleep wakening
- Increased cramps
- Onset of night sweats, in particular premenstrually
- New or markedly increased migraine headaches
- New/increased premenstrual mood swings
- Weight gain without changes in exercise or eating
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987489/
Those are some symptoms that can crop up before the roller coaster...maybe years before.
Look...symptoms can start really early.
In fact:
Nearly 44% of women start having VMS approximately 11 years before their final menstrual period.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459071/
VMS is short for vasomotor symptoms tied to hormone shift such as hot flashes, etc.
Doctors can look at hormone panels as certain hormones will start to change (FSH, activin, inhibin, etc) but that's not always a definitive sign in all women.
Perimenopause is in full force when we have 12 months without a period.
Technically, it should end after that run and then menopause is in effect.
Perimenopause is the transition over to menopause primarily described by 12 months without a period and the flux of estradiol.
What about those symptoms? Do they get better or worse?
Are the symptoms worse in perimenopause or menopause
Each woman is different of course and many systems play into the severity and duration of symptoms.
- Neurotransmitters
- Endocannabinoid system (balancing act)
- Immune system
- Hormone system
- Epigenetic aging
- Early trauma, stress, or infection
Obviously, lifestyle choices such as smoking, drinking, exercise, drug use, etc will play a role in all the above...especially the epigenetic aging piece.
For example:
Factors that are toxic to the ovary often result in an earlier age of menopause; for example, women who smoke experience an earlier menopause
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4539866/
This is essentially the aging of our DNA...a real "age" separate from our chronological age.
The symptoms during perimenopause may be more debilitating or off-balance compared to menopause.
For example, hot flashes.
Hormone replacement therapy has been shown to virtually eliminate them.
That being said...
However, estrogen reduction alone does not explain the occurrence of HFs because there are no relationships between these symptoms and plasma, urinary, or vaginal [20] levels of estrogens, nor are there differences in plasma levels between women with and without HFs
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612529/
That's a puzzle.
Estrogen replacement helps with symptoms but symptoms are not tied to estrogen levels.
The only thing left is the "change" in estrogen.
The flux of hormones, especially estradiol, occurs during perimenopause...not menopause.
Looking at the graph here, you can see that levels are fairly flat once menopause is in effect.
https://www.zrtlab.com/blog/archive/mood-menopause-perimenopause/
So really the symptoms of perimenopause and menopause are quite different even if the same levers are being pulled:
- Perimenopause - erratic ups and downs in estradiol drive serotonin and other pathways
- Menopause - greatly reduced levels of estradiol reduce serotonin and other pathways
Serotonin spiking up is very different from a gradually reducing level.
Both equally bad but in different ways.
Just check out CBD and serotonin syndrome (too much serotonin) to see how bad that can be.
On the other hand, check out CBD and serotonin to see what happens when it goes down!
Serotonin directly drives BDNF, our brain's fertilizer as well which is the key to loss of hormones and dementia risk longer term.
Perimenopause can be very extreme (especially for the 25% of women with severe transitions).
As for menopause, estrogen is intimately tied to vitality.
We don't just mean hair, skin, and bones (although, all directly thrive with estradiol).
Afterall, estradiol is a growth factor in the body (see estradiol review) depending on which receptor (alpha or beta).
For example, interesting research looked as estradiol's neuroprotective function following stroke:
Our results demonstrate that deletion of ERα completely abolishes the protective actions of estradiol in all regions of the brain; whereas the ability of estradiol to protect against brain injury is totally preserved in the absence of ERβ.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC29363/
The brain and heart are equally under its direct control.
First, the brain:
Among findings, surgical menopause increased the risk of dementia or cognitive impairment by 45 percent.
Check out CBD and dementia to learn more.
In fact, we can look at women who have their ovaries removed (the main source of estradiol and progesterone) to see the effects.
These symptoms occur almost immediately and can persist for decades. Untreated, symptoms such as hot flashes, sleep disturbance, fatigue, decreased sexual desire, anxiety and depressed mood often have a major impact on quality of life, capacity to function, and disease risk
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5248494/
Establishing that it was primarily a loss of estradiol following the surgery, the effects are widespread:
The Mayo Clinic Cohort Study of Oophorectomy and Aging reports that following bilateral oophorectomy risk is increased for all-cause mortality (28%), coronary heart disease (33%), stroke (62%), cognitive impairment (60%), parkinsonism (80%), osteoporosis and bone fractures (50%), sexual dysfunction (40-110%), and, possibly, glaucoma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5248494/
So when your doctor doesn't check your hormones and instead, writes a script for SSRI's or benzos...get very angry. Very angry.
Check out Siberian Rhubarb review if you're afraid of estradiol replacement.
Those disease risks are more from longer-term loss of hormones. That's menopause!
Why do some women get hit so hard with perimenopause?
They still don't know why some women get hit so hard while others don't but you can bet it's at the intersection of the above systems.
There are some clues.
Just last week, a study found that women with hypertension when pregnant may have more difficult perimenopause:
Compared with nonparous women, the researchers reported a difference of 2.34 (95% CI, 0.67-4.01) in total menopausal symptom scores for women who had a hypertensive disease of pregnancy (P =.006).
The benchmark they used was "somato-vegetative" symptoms which mean so severe, that you can't function.
And estrogen's role in hypertension or preeclampsia during pregnancy?:
A close link between estrogen dysregulation and PE occurrence might validate estrogen levels as a biomarker but could also reveal a potential approach for the prevention or cure of PE.
https://academic.oup.com/edrv/article/38/2/123/3061617
Another fascinating piece is that women with fairly calm cycles earlier in life may be hit harder in perimenopause.
That was me! I saved it all up for the finale!
What research is saying is this…
It's the change (spike or drop) in estradiol that causes most of the severe perimenopausal symptoms.
Remember...it's estimated that 25% of women will experience perimenopause that's severe.
For one example:
studies estimate that 26–33% of women develop clinically significant depressive symptoms during this time
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5113718/
And on the extreme side:
Rates of full-blown major depressive disorder during the menopause transition range between 12 and 23%
That's millions of women!
Of course, SSRI's are the go-to remedy with all their issues (see CBD versus SSRI for serotonin).
While you're at it, check out CBD and perimenopause depression here to learn the nuance of depression during this time.
After the deep dive into estradiol supplementation, we had to fully investigate Siberian Rhubarb (the ERr 731 extract version). It's pretty amazing!
Now, since we have personally suffered at the hands of perimenopause and the doctors were soooo out to lunch...we want to go DEEPER.
Why did my mom get through with hot flashes while I came unglued (after decades of being very level...in case you're wondering)?
This is where it gets interesting and we're going to have to break it out for an entire article to really get at it.
They ran a genetic study to see if certain genes were tied to rough perimenopause.
Association of genetic variation in the tachykinin receptor 3 focus with hot flashes and night sweats in the Women’s Health Initiative Study
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5327841/
You're probably thinking...tachy WHAAT??
Stay with us. It's a winding road but VERY interesting.
This is a family of chemicals in the nervous system with primary residence in the hypothalamus.
A very important brain area for our discussion as we'll see below.
There are three main players in this family:
- Neurokinin B
- Dynorphin
- Kisspeptin
Great names. Better effects.
Let's take hot flashes, the most common symptom of perimenopause and menopause with over 80% of women affected.
Neurokinin 3 receptor antagonism rapidly improves vasomotor symptoms with a sustained duration of action
Well, that's interesting!
And what is dynorphin? It's a naturally occurring opioid that governs the pain threshold. (check off one more big symptom of perimenopause).
And kisspeptin?
Oh...it just controls GnHR, the finger on the trigger of FSH, in the hypothalamus:
Gonadotropin-releasing hormone is released from the hypothalamus to act on the anterior pituitary triggering the release of luteinizing hormone (LH), and follicle-stimulating hormone (FSH).
https://en.wikipedia.org/wiki/Kisspeptin
To circle all the way back around, FSH is the hormone that's in a cat-and-mouse roller coaster with estradiol during perimenopause!
It's also the main "signal" that they test to see if a woman is in menopause.
Neuropeptide B really looks fascinating...one because of the genetic tie-in but also because of its effects on the rest of the chain:
Thus, we have proposed a model in which NKB feeds back to the KNDy neuron to shape the pulsatile release of kisspeptin, and hence GnRH, in a mechanism also dependent on the sex steroid level.
https://www.ncbi.nlm.nih.gov/pubmed/23550013
"Pulsatile" just means in waves of release. Remember how estradiol will spike and drop?
Also, remember how it was just found that women who have hypertension or preeclampsia are at a higher risk for rougher perimenopause?
The first NKB studies done attempted to resolve why high levels of the peptide may be implicated in pre-eclampsia during pregnancy
https://en.wikipedia.org/wiki/Neurokinin_B
Hmmm. Genes. Prior issues during pregnancy. Up-stream control of hormone that governs estradiol and FSH.
What about all the heart-related symptoms:
- Raised blood pressure
- Skipped heartbeats
- Feeling your heartbeat more forcefully (scary and weird effect)
Oh, just this...
Tachykinins also regulate vascular tone and blood flow, although differences between species and between different vascular beds make this a highly complex area of research
https://www.ncbi.nlm.nih.gov/pubmed/16918331
Highly complex, I bet!
It was this "family" of effects that sent me into a medication tailspin with the doctors!
Blood pressure meds, heart meds, heart scans, heart monitors, etc.
That wonderful story is here.
The last symptom I have is pain in my heels. After multiple doctors, MRI's, bad diagnosis, boots, inserts, and various balms, it's looking more and more like regional complex pain syndrome.
Look at this list of symptoms from tachykinin dysregulation:
Cardiovascular effects of tachykinins and neurokinin receptors may be important therapeutic targets in diverse disorders such as pulmonary edema, hypertension, pre-eclampsia, complex regional pain syndrome type 2, and chronic inflammatory diseases such as arthritis
Regional pain syndrome. Great.
The connection between estrogen levels and pain may find partial explanation further upstream:
The greatest reports of pain symptoms appear to occur at times of low or rapidly falling estrogen levels and the use of the combined oral contraceptive pill (COCP) to give a more constant hormonal level can improve these symptoms.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589942/
This then points us to the hypothalamus.
It's an almond-sized brain area deep in the nethers of the old "reptilian" brain.
We share it with all animals.
It acts as a master control switch between our nervous system/brain and our hormone systems.
If you read through its list of activities, it might as well be our perimenopausal symptoms:
https://en.wikipedia.org/wiki/Hypothalamus
A recent study where they were able to REVERSE the epigenetic age of people by focusing on growth hormone release and the thalamus is intriguing as well.
The growth hormone is a key determinant of biological aging in general.
Do hormones affect this?
Specifically, GH output declines more with aging in young men than premenopausal women and more when aging is accompanied by abdominal visceral adiposity, hyperinsulinemia; and oestrogen and testosterone (acting via oestrogen) deprivation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3920108/
Estrogen deprivation hurts growth hormone (which leads to aging).
Let's bring it all together before looking at ways we can do here:
In addition, menopause is accompanied by hypertrophy of neurons in the infundibular (arcuate) nucleus expressing KiSS-1, neurokinin B (NKB), substance P, dynorphin and estrogen receptor α (ERα) mRNA.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2632595/
Hypertrophy is "shrinking". If you read our CBD for elderly anxiety, shrinking (loss of BDNF) and retrenching is a critical piece of age-related brain issues (anxiety, depression, etc).
That crazy word "infundibular arcuate nucleus" is just a sub-section of the...hypothalamus!
Just on the surface level, does estrogen have any effect in this area?
Estrogen has multifaceted effects on the hypothalamus that regulate a number of homeostatic functions including reproduction, temperature, energy balance, stress, and motivated behaviors.
https://www.ncbi.nlm.nih.gov/pubmed/16112267
Okay...just checking. And we're losing estrogen. Or seeing it go haywire during perimenopause.
To wrap this all up, a study looked at how symptoms were tied to a lack of sensitivity in the hypothalamus.
Basically, the typical controlling mechanisms (which we showed are the tachykinins above) are not responding accordingly.
Their results:
Our findings are compatible with hypothalamic-pituitary insensitivity to estrogen in aging perimenopausal women.
https://jamanetwork.com/journals/jama/fullarticle/200055
Look...we took you far astray but we wanted to let you know why I (and maybe you) had such a bad perimenopause.
Someone has to do this!
So what can we do about it?
How do I get through perimenopause and menopause successfully (translated...with sanity intact)
When I started this process, it was very dark indeed.
I've tried dozens of different supplements, medications, and even gadgets.
I'll leave the benzos, SSRIs, and other medications to other sites but we dove deep in them here:
How SSRIs work
Benzos versus CBD
Here's are perimenopause toolkit:
Front and center are bioidentical hormones and/or Siberian Rhubarb (ERr 731).
Progesterone was instrumental in getting my life back followed by estradiol. We looked at the whole oral versus topical issue. The go-to's:
- Estrace - bioidentical oral estradiol (in the morning)
- Prometrium - bioidentical oral progesterone (before bed)
The Siberian Rhubarb came later after much research but I use it as a protective measure to the growth focus of estradiol.
Check out the full review on Siberian Rhubarb for perimenopause or Estradiol for Perimenopause.
Pregnenolone might be a good workaround for progesterone. Check out the review here. Its effects on aging are a bonus!
Work with a doctor or better yet, a naturopath….as long as they will work WITH you.
Other key aids along the way:
- Magnesium - any of the "ates" such as theornate or glycinate. The Super Mag from GNC had an immediate effect
- Vitamin D and lots of it (get tested). Vitamin D is deficient in many women and it's critical to governing Serotonin (the target of SSRI's) and protecting from estradiol's pro-growth effects
- B vitamins - especially folate, B12, and B6 with methylated versions being key for many women
- Chromium picolinate - may help support the hypothalamus
- Mindful meditation and exercise for stress response (see CBD, meditation, and exercise here).
I get the Siberian rhubarb, pregnenolone, and supplements here.
Then there's CBD to smooth out the edges of perimenopause.
Take a look at CBD for perimenopause anxiety and CBD for perimenopause depression for in-depth looks at the pathways.
It affects the same pathways as benzos (GABA) and SSRIs (serotonin but really BDNF) without the nasty addiction and rebound effects.
A big part of perimenopause response is a stress response and that's under the direction of the endocannabinoid system.
Just look at this study here:
Greater estradiol variability across the 14 months predicted greater depressive symptoms at month 14, though only in women reporting a higher number of VSLEs at baseline
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4764412/
The key term there...VSLE. Very Stressful Life Events.
The fluctuation in hormones (estradiol) is already stressful when so many systems rely on it for functioning correctly.
Combine this with stressful life events (my teenagers perhaps) and you're shaking the apple cart.
Check out CBD and stress or CBD and neuroinflammation to see how targeted CBD can be.
Maybe, more importantly, is how extensively involved the endocannabinoid system is in the hypothalamus:
Second, receptors and metabolic enzymes of the endocannabinoid system are localized extensively on structures in the hypothalamic-pituitary-gonadal axis
https://academic.oup.com/endo/article/153/3/1016/2423624
There's a great deal of research on CBD and many of the symptoms tied to perimenopause which speaks to this crossover.
A great deal of this is its effect on serotonin which estradiol is in direct control of.
For example:
Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6319597/
Allodynia is all-around body pain.
The key word there is "modulate".
Not increase or reduce. Balance. That's the primary role of the endocannabinoid system and it's one under serious duress during perimenopause.
Next up...there's interesting research on specific acupuncture points tied to the hypothalamus function.
You can get a TENS unit on Amazon here and apply it to those points.
The primary ones for pain:
- ST36
- GB34
And for hypothalamus function including hormones:
- BL23
- BL18
- LR14
- GB25
- GB24
- LR13
- DU14
- ACR
Just google "acupoint" followed by the name above for location.
This hopefully gives you some guidance and maybe even marching orders going into the perimenopause transition to menopause.
They're VERY different and now you know why.
Now...go explain it to your doctor.
This glimpse into perimenopause is just the beginning. 'Dre's Story' offers our complete, research-rich journey into hormones, tools to feel better, and safety. The full Perimenopause Toolkit with new additions can be found Here. Please review so other can learn. Feeling better starts with understanding what is happening.
Get specific links for CBD and Perimenopause symptoms and questions here.
Related Research:
Why is perimenopause so hard for some women
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.