The Immune System is the New Frontier for Mental Health

A great deal of the new research is finding interesting connections between the immune system and mental health issues.
Even cutting research on psilocybin recently found that longer-term effects were hinged on changes in genes tied to inflammation or immune function.
We'll get into all of that.
First, we need to stop thinking of the immune system as just a way to fight infection.
There's a whole other side to it which deals with cellular birth/death cycles and even the ever-changing architecture of the brain itself.
Every mental health issue we've studied (see CBD and mental health) has an inflammation pathway involved.
From anxiety to depression and schizophrenia to dementia….the immune system is in play.
Don't take our word for it:
Far from being specific to any one mental illness, or a sub-population within a mental illness, inflammation turned out to be a common denominator and likely risk factor for every manner of psychiatric disturbance, from schizophrenia to obsessive-compulsive disorder, from mania to depression
https://www.psychiatrictimes.com/view/introduction-inflammation-connection
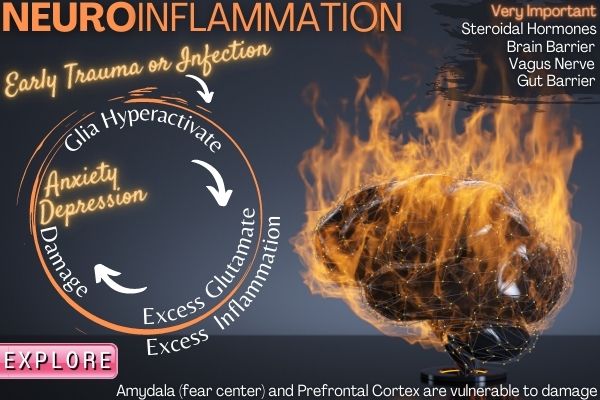
Especially when primed early by infection or trauma!
We'll slow walk you through the process of how this whole system can get imbalanced and then most importantly, look at ways to calm brain inflammation.
This is the most exciting new avenue in actually reversing issues in decades!
These are the topics we'll cover:
- The immune system's other job
- Brain inflammation and mental health
- The brain's immune system players
- Immune system and different types of mental illness
- Trauma and stress effects on the immune system and mental health
- The gut and brain blood barrier
- The gut-brain axis via the vagus nerve
- Oxidative stress and mental health
- Tools to calm brain inflammation for mental health
Let's get started.
The inflammation and mental health connection
Yes, our immune system's primary task is that of recognizing and removing foreign entities.
That plays into our discussion on mental health partially since inflammation (the immune's main weapon) carries with it, collateral damage to healthy tissue.
In fact, studies have looked at increasing inflammation to see if it could lead to mental health issues.
It did!
Besides the observation in patients suffering from malignancies or chronic inflammatory diseases, experimental data in healthy humans confirmed that cytokines, particularly TNF-α and IL-6, induce depressed mood, anxiety, and memory impairment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181623/
This is fascinating...just boosting cytokines (the little assassins of inflammation) can cause anxiety and depression.
Why? Why would the body do this or is it just an unintended consequence?
A little bit of both.
First, there's the whole tryptophan starvation angle.
If the immune system thinks we're under attack, the body will start to block tryptophan conversion into serotonin, our primary mood manager and governor of all things surrounding human behavior.
This is because viruses and bacteria use that same tryptophan (a very basic amino acid) to make more of themselves.
The body is attempting to starve that production but in doing so, serotonin also takes a hit.
Check out our review on tryptophan and stress to learn more or research the tryptophan/serotonin process.
Serotonin is the target of SSRIs (anti-depressants) so we see the clear angle.
SSRIs boost serotonin but they build tolerance over time (see CBD versus SSRIs).
It gets better.
Serotonin directly drives BDNF, our brain's fertilizer.
If you dig into how SSRIs really work till tolerance kicks in, it mainly comes down to BDNF to repair, replenish, and grow brain connections.
BDNF is the star of the mental health show (see CBD and BDNF or brain repair).
This whole pathway is starved out in the presence of infection/inflammation.
Here's the rub….the immune system is a one-trick pony, albeit with many moving pieces.
It responds to psychological stress and trauma much the same way it responds to bacteria and viruses.
Psychological stress triggers inflammatory activity and affective-cognitive changes that play a critical role in the onset, maintenance, and recurrence of depression.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6491771/
Goodness...so the immune system responds to being ostracized or abused similarly to getting the flu.
We'll go deeper into this in the trauma section below since it's so critical.
Just keep the following on your radar:
- Infection
- Stress (chronic or acute)
- Trauma
- Early abuse, infection, trauma (even in utero)
We'll look specifically at key mental health issues and inflammatory markers to further link everything but let's turn to the other role of the immune system in the brain.
The immune system's other job
Talk about wearing two hats.
Fight infection and while you're at, be in charge of the brain's architecture that's changing by the second.
Yes, in the brain, the immune system manages the growth, change, and even death of physical connections and pathways.
That's as big as it sounds.
In fact, infection or trauma during key periods of brain development (3rd trimester, etc) can have profound impacts later in life.
The microglia act like generals of the brain's immune system and they coordinate this other process as well:
Microglial cells, the brains equivalent of macrophages, appear central to dendritic pruning and neural plasticity while MHC proteins central to self/non-self distinctions play a critical role in early neural development.
https://jnnp.bmj.com/content/84/9/e1.33.short
Neural plasticity. A fancy way to say molding and shaping the brain.
If microglia are not functioning correctly, the repercussions are pronounced:
Aging-, stress- or disease-associated alterations of microglia may cause impairment of these beneficial physiological processes and result in neuroinflammation, neurodegeneration, synaptic loss, behavioral changes and/or increased susceptibility to mental diseases in later life stages
https://www.psychiatrictimes.com/view/microglial-involvement-psychiatric-diseases
See stress and infection as key drivers of imbalance?
We have a whole review on microglia or neuroinflammation which dives deeper into this.
The effect of this imbalance can be felt across the spectrum:
- Developmental diseases - schizophrenia, autism, bi-polar, etc
- Developing diseases - anxiety, depression, OCD, dementia, etc
Developmental diseases can result from stress, infection, trauma during key windows of brain development.
The development can occur throughout life or have an initial kickoff.
Before we dive into specific mental health issues, let's introduce the players so we know what to track.
The brain's immune system players
We need at least a basic introduction.
- Microglia - the main managers of immune response in the brain
- Cytokines - a virtual zoo of specific inflammatory players
- Astrocytes - manage the all-important blood-brain barrier
- Oligodendrocytes - supports and protects nerves and neurons
- Glutamate and BDNF - the brain's "gas pedal" and fertilizer (respectively); levels are managed by microglia
The immune system is incredibly complicated. Researchers finally discovered that amyloid-beta particles (prevalent with dementia) are a specialized type of cytokine that targets bacteria (hint hint...autoimmune). See CBD and dementia.
A quick lay of the land.
Microglia
This network of "sentinels" starts to form 9 days after conception and stays with you for life.
The microglia have key roles that directly affect brain function:
- Balances and manages brain cell birth/death levels - key for pruning (think around age 2, puberty, and early adulthood).
- Manages levels of oligodendrocytes - key for nerve protection and brain-blood barrier
- Remodels ongoing brain pathways - key for addiction, mental health, and repair
To summarize:
Taken together, functional microglia are essential for synaptic formation, maintenance and plasticity, as well as remodeling of neural networks in response to learning and environmental challenges.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5758507/
So...engineering, construction, and demo in the brain.
The key there is "learning and environmental challenges".
Within that broad scope, you can have "bad" learning. Trauma. Abuse. Addiction (a chemically induced type of learning). Infection.
Microglia may be key to early triggers of the immune response:
Enduring fevers or maternal infections during pregnancy, and physiological injuries at birth (e.g., infection, hypoxia-ischemia and trauma) increase the risk for autism, attention deficit and hyperactivity disorder, and schizophrenia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5758507/
The glutamate piece is fascinating.
Excess glutamate is a known issue with mental health. Glutamate can be toxic to nerves and connections in the brain.
For example:
Glutamate and microglia activation as a driver of dendritic apoptosis: a core pathophysiological mechanism to understand schizophrenia
https://www.nature.com/articles/s41398-021-01385-9
Basically, hyperactive microglia release too much glutamate which kills nerves and their connections.
See CBD and glutamate. We'll look at tools to protect from excess glutamate below.
What about cytokines?
Cytokines and mental health
When looking at common mental health issues, there's clearly a connection:
Results showed that in men, higher levels of TNF-α were associated with more severe psychiatric symptoms. Further, age moderated the association between TNF-α, as well as IL-6, and stress, and exploratory stratified analyses revealed significant associations in subgroups
https://www.sciencedirect.com/science/article/pii/S2666354620300107
A study looked at mood specifically after the introduction of an endotoxin that would boost cytokines. The results on cytokines:
increased the circulating levels of tumor necrosis factor α (TNF-α), soluble TNF receptors, interleukin (IL)-6, IL-1 receptor antagonist, and cortisol
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/481767
And resulting mood…
After endotoxin administration, the subjects showed a transient significant increase in the levels of anxiety (effect size [ES] = 0.55) and depressed mood (ES = 0.66).
We'll look at specific cytokine changes by disease below.
Let's turn our attention to the protective sac around the brain and the astrocytes that manage it.
Astrocytes and mental health
If microglia are the management of the brain's architecture and immune response, astrocytes are the labor.
They have varied roles from supplying nutrients to neurons, detoxification, energy balancing, and repair.
But their star role (in our eyes) is that of the blood-brain barrier.
Think of the brain as very very expensive real estate with a strict security border.
The BBB is critical these days since most diseases (even mental health diseases) are starting to display aspects of autoimmune.
What is triggering the brain's immune system to hyperactivate?
Bacteria, viruses, and more can gain entry into the blood via the gut and mouth.
If the blood-brain barrier is broken, they can then enter the brain and trigger the immune response.
In fact, studies on schizophrenia, autism, and more show issues around this barrier:
Increased permeability of the BBB appears to be a common factor in these disorders, leading to increased infiltration of peripheral material into the brain culminating in neuroinflammation and oxidative stress.
https://pubmed.ncbi.nlm.nih.gov/29966749/
Inflammation and oxidative stress...enemies of the precious real estate in our skull.
It's also anxiety, depression, and more common issues.
Recent experimental data indicate that anxiety and depressive-like behaviors occurring as a result of stressful situations can cause blood-brain barrier (BBB) dysfunction, which is characterized by inflammation and leakage.
https://pubmed.ncbi.nlm.nih.gov/32333258/
Check our review on autoimmune or the blood-brain barrier.
We'll also look at the backdoor channel between the gut and brain via the vagus nerve below. Stay tuned.
Let's turn to one more piece.
Oligodendrocytes and mental health
We'll start with the teaser:
Low density and reduced expression of oligodendrocyte-specific gene transcripts in postmortem human subjects points toward decreased oligodendrocyte function in most of the major mental illnesses
https://www.nature.com/articles/tp201234
We know from above that microglia manage oligodendrocytes.
We did a massive review on stress and mental health here. There's an interesting intersection between stress response and oligodendrocytes.
After mice were exposed to stress (think trauma, etc), there was a marked difference in which type was able to handle the stress:
the research team detected fewer mature oligodendrocytes and irregular myelin coverage in the medial prefrontal cortex -- a brain region that plays a critical role in emotional and cognitive processing -- in the susceptible mice. In contrast, healthy numbers of oligodendrocytes and myelin were detected in resilient mice.
https://www.sciencedaily.com/releases/2019/08/190813080212.htm
So resilience….a key piece of the mental health landscape.
The key to oligodendrocytes in the myelinization or the sheathing around neurons and their connections.
One final piece...not an immune player but a generalized brain player that's managed by the immune system.
Glutamate and BDNF and immune response
These are not immune system players but the microglia manage their levels.
They are critical to a functioning brain and all over the map of mental health.
We have a big review on glutamate (here) and BDNF (here) but a few key takeaways.
Glutamate is our brain's "gas pedal". Everything that runs is driven by glutamate receptors. Even GABA, its counterpart ("Brake pedal" and target of benzos).
We have fail-safe systems to keep glutamate at a healthy level since it's toxic to nerves when too high.
Glutathione, magnesium, GABA, glycine, and others all work to keep it in check.
Otherwise, it's like red-lining an engine...it will burn it out (neuron death or dysfunction).
We have big reviews on each of those and they'll figure into how we push back below.
Here's the connection with the immune system:
combination of failed clearance and exaggerated release of glutamate by glial cells during immune activation leads to glutamate increases and promotes aberrant extrasynaptic signaling through ionotropic and metabotropic glutamate receptors, ultimately resulting in synaptic dysfunction and loss.
https://www.nature.com/articles/npp2016199
Translation, please!
Essentially, too much glutamate released by microglia (immune sentinels) causes neurons not to function correctly and even die off!
Remember that microglia can be set off by stress, trauma, infection, etc.
The net result if too much or chronic:
Glutamate released by activated microglia induces excito-neurotoxicity and most likely contributes to neurodegeneration in numerous neurological diseases including ischemia, inflammation, epilepsy and neurodegenerative diseases.
https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1759-1961.2009.00001.x
Glutamate is essential but too much is like scorched earth.
The effects of this run through every mental health issue. We'll look at how to address this below.
That's the damaging side...what about the repair piece?
BDNF! Brain derived neurotrophic factor.

If you're interested in mental health, addiction, and brain repair, this is your new best friend.
It turns out that astrocytes are major regulators of BDNF!
Surprisingly, we found that astrocytes are the main recipient of neuronally expressed BDNF.
https://www.biorxiv.org/content/10.1101/255935v2.full
Remember how astrocytes were involved in repair? We can't tell you how important this is.
BDNF is THE key to repair and mental health function.
As an example, the two main triggers for relapse with addiction?
- Stress
- BDNF levels
Again, we'll look at how to boost this below.
Okay...we've introduced some key players.
Let's now dive into the main mental health issues and see how they are affected.
Brain inflammation and mental health
We'll focus on a few key broad-spectrum mental health issues. Message us via chat box below regarding research on specific issues and we'll send that over (or do the deep dive):
- Anxiety and inflammation
- Depression and inflammation
- Schizophrenia and inflammation
- Dementia and inflammation
We have a mix of issues tied to imbalance, developmental, and deteriorating effects.
Let's get started.
Anxiety and inflammation
We have a deep dive on anxiety and neuroinflammation as well as the pathways of anxiety.
There are clear ties to the immune system and inflammation with anxiety.
It's important to understand the daisy-chain effect of stress on inflammation.
Anxiety is a nice example of this.
Studies have shown that elevated levels of interleukin-6 are consistently found in individuals suffering from mood disorders like depression and anxiety.
Okay...IL6 is a common cytokine...immune responder.
IL6 is involved in the ramp-up response to infection or other stresses.
Remember...the immune system has one response whether it's an infection, stress, trauma, etc.
For example:
One important immunological effect of short-term stress is an induction of an increase in concentrations of circulating cytokines (such as IL-6, as also shown in our data).
https://www.nature.com/articles/srep23008
Okay...so stress directly ramps up the immune response.
That's okay (getting ready for battle) but if chronic or traumatic, it leads to a constant state of brain inflammation.
In the short term, this wears down GABA (our brake pedal) but longer-term, it actually remodels our brain...especially the circuits around fear response (amygdala and prefrontal cortex).
Furthermore, anxiety- and depression-like behaviors induced by chronic mild stress57 or postnatal stress60 are associated with increased microglial ‘activation’ in the hippocampus, and acute unpredictable stress increases microglia density in the DG of mice
https://www.nature.com/articles/s41398-020-00942-y
You can't be on the edge of battle forever!
The reason we're even looking at this (we being CBD researchers) is that the endocannabinoid system is tied to re-balancing these key systems after periods of stress.
See CBD and microglia to learn more.
But even in the short term, effects of inflammation on GABA, our key calming neurotransmitter are pronounced.
In fact, we can look at animal studies that focus on the role of inflammation on GABA function after an antibiotic:
Minocycline ameliorates anxiety-related self-grooming behaviors and alters hippocampal neuroinflammation, GABA and serum cholesterol levels in female Sprague-Dawley rats subjected to chronic unpredictable mild stress
https://pubmed.ncbi.nlm.nih.gov/30703398/
This is fascinating...by calming brain inflammation, they see GABA function change in a key area of the brain tied to mood.
Studies have followed the links from stress to brain inflammation to resulting anxiety or depression:
Stress-Induced Microglia Activation and Monocyte Trafficking to the Brain Underlie the Development of Anxiety and Depression
https://pubmed.ncbi.nlm.nih.gov/27352390/
This creates a feedback loop.
In fact, researchers can introduce cytokines and cause the whole stress response system to cascade down:
Administered cytokines stimulate the expression and release of corticotrophin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and cortisol, all of which are altered in depressed patients
(above link).
Goodness...you trigger stress by introducing cytokines and stress causes an increase of cytokines.
Check out CBD and stress response to learn more.
So...chronic inflammation will drive stress pathways. That's going to eat up GABA (our calming neurotransmitter), allow glutamate to run amok, and change the architecture of the brain (especially the hippocampus and amygdala-prefrontal cortex interface) longer term.
Hello Anxiety!
We can understand how trauma might break this system and chronic stress might wear it down, but we'll look at early infection/trauma later to see how "trait anxiety" - lifelong anxiety can be primed via the immune system below.
Let's turn to depression.
Depression and inflammation
You can think of depression as a disintegration of brain areas and neurons.
So what's the connection with SSRIs when they do work (about 30% of the time till tolerance builds up) or psilocybin?
The true star behind those curtains is BDNF...our brain's fertilizer. It's rebuilding, repairing, and replenishing.
As we showed in our How do SSRIs really work review, when BDNF is turned off, the neurogenesis (brain repair/growth) goes away as does the anti-depressant effects.
Psilocybin is a massive boost of neurogenesis and synaptogenesis (growth of connections).
Here's the curious piece...a brand new piece of research showed that the genes affected by psilocybin which were responsible for the longer-term effects actually governed...immune response!
Immune-related genes constituted the largest group of genes impacted one week after psilocybin administration, suggesting that the long-lasting effects of the psychedelic substance might be related to neuroinflammation.
As for cytokines, one stands out:
There were significantly higher concentrations of TNF- a p .00001), weighted mean difference (WMD) (95% confidence interval) 3.97 pg/mL (2.24 to 5.71), in depressed subjects compared with control subjects
https://pubmed.ncbi.nlm.nih.gov/35782448/
IL6 was also elevated but TNF-a was much higher.
TNF-alpha is interesting...essentially is a signaling for cellular suicide:
Tumour Necrosis Factor alpha (TNF alpha), is an inflammatory cytokine produced by macrophages/monocytes during acute inflammation and is responsible for a diverse range of signaling events within cells, leading to necrosis or apoptosis.
https://pubmed.ncbi.nlm.nih.gov/10891884/
If a cell goes awry, TNF-alpha is one of the immune players to start the process of removing it.
It's a major sign of heightened inflammation since we typically find it in the acute phase (initial response to infection).
And the immune response sentinels...microglia? :
studies revealed the activation of the brain immune cell microglia in depressed patients with a greater magnitude in individuals that committed suicide, indicating a crucial role for neuroinflammation in depression brain pathogenesis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4681811/
So...more damage.
And less repair:
BDNF was found decreased in depressed patients and in stressed animals (Dwivedi, 2009).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4681811/
The stress part is key...serotonin gets depleted by stress and serotonin drives BDNF!
Check out our full review of CBD and depression.
Let's turn to a developmental illness.
Schizophrenia and inflammation
We have a massive review of the pathways surrounding schizophrenia here.
The end result is an imbalance of dopamine in two separate brain areas.
But..neuroinflammation lies just below the surface!
First, the cytokines:
Exploring detailed data on immune-inflammatory disturbances in SZ reveals that IL-6 is one of the most consistently disturbed cytokines. Other cytokines, including IL1, TNF, and IFN, are also disturbed in schizophrenia.
https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00160/full
IL6 again. IL6 is a big responder to inflection...bacterial, viral, and the like.
TNF is the same as depression...tied to removing infected cells.
All of the cytokines above speak of a body ramping up for fighting infection...or primed for trauma/stress!
We can then look at associated risks and genes tied to risk:
A large epidemiological study clearly demonstrated that severe infections and autoimmune disorders are risk factors for schizophrenia. Genetic studies have shown a strong signal for schizophrenia on chromosome 6p22.1, in a region related to the human leucocyte antigen (HLA) system and other immune functions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612505/
Goodness. Autoimmune (see our CBD and autoimmune review) is generally driven by bacteria/viruses escaping our gut, mouth, etc and triggering chronic inflammation to combat these interlopers throughout the body.
Think of that as a low-level infection.
Maybe more interesting are the anti-inflammatory medications such as COX2 inhibitors.
The patients receiving celecoxib add-on to risperidone showed a statistically significantly better outcome than the patients receiving risperidone alone; the clinical effects of COX-2 inhibition in schizophrenia were especially pronounced in cognition
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612505/
But it's not just this class but all things that calm inflammation:
Other anti-inflammatory agents have been explored, including hormonal therapies, antioxidants, omega 3 fatty acids, and minocycline, showing significant effects for reducing total, positive, and negative score symptoms and general functioning.
https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00160/full
Schizophrenia is tricky. There are two classes of symptoms (positive and negative) that reflect dopamine imbalance in two different brain areas respectively.
The fact that reducing inflammation affected both classes speaks to a systemwide upstream effect.
We'll go into where this might originate later. This is a fascinating piece.
Let's turn to degenerative brain diseases with the primary one on everyone's mind.
Dementia and inflammation
We did a deep dive on dementia and CBD here.
Those amyloid plaques?
They're actually uncommon little cytokines that exist in our brain to attack bacteria.
Recent studies have found that beta-amyloid has antiviral and antimicrobial properties, suggesting a potential link between the immune response against infections and the development of Alzheimer's disease.
https://www.genengnews.com/news/researchers-reveal-how-immune-response-plays-a-role-in-alzheimers/
There's also the connection between age and dementia.
It's now well established that systemic inflammation increases as we age. Nicely called inflammaging.
Scientists can play with inflammatory pathways and directly affect the progress of genes:
a plethora of studies have demonstrated that modulating immune system specific proteins impacts the development of AD pathology in various experimental systems, suggesting that the immune system directly impacts pathology.
https://www.frontiersin.org/articles/10.3389/fnagi.2019.00337/full
You would expect microglia to be involved since they're running the brain's immune show.
in-vivo detection of increased [11C](R)- PK11195 binding in Alzheimer-type dementia, including mild and early forms, suggests that microglial activation is an early event in the pathogenesis of the disease.
Microglia activation.
A look at brains of postmortem dementia sufferers confirms this:
There was a positive correlation between the numbers of activated microglia and LB in different brain regions. This study demonstrates the presence of significant inflammation in DLB, even in the absence of AD pathology.
https://n.neurology.org/content/55/1/132.short
So inflammation comes first. Disease follows suit.
The bigger clue is this.
Non-steroidal anti-inflammatory drugs, which inhibit the cyclooxygenase enzymes COX-1 and COX-2, reduce the risk of developing Alzheimer’s disease in normal ageing populations. This preventive effect coincides with an extended preclinical phase that spans years to decades before onset of cognitive decline.
https://academic.oup.com/brain/article/139/7/2063/2464317
Remember that inflammaging?
A slow-rolling state of inflammation.
Okay...we could go on and on along these lines and just about every mental health issue but let's turn to the more fascinating piece.
Trauma and stress effects on the immune system and mental health
Again, we did a giant review on how trauma, especially early in life during key points of development, can increase risk for mental health later.
But why?
Hello, immune system.
The immune system can be primed by early exposure to infection or stress.
This can even be an infection in utero (3rd trimester).
Let's look at some of the pathways/issues above to punch through this.
We'll cover these areas:
- Early trauma, immune, and serotonin
- Early trauma, immune, and GABA/glutamate
- Early trauma, immune, and anandamide
- Early trauma, immune, and brain inflammation
- Early trauma, immune, and anxiety
- Early trauma, immune, and depression
- Early trauma, immune, and schizophrenia
- Early trauma, immune, and dementia
Okay...remember...for trauma, it could be infection, chronic stress, acute (traumatic) stress.
The immune system responds to each very similarly. We'll go through these quickly.
Early trauma, immune, and serotonin
Early trauma dysregulates serotonin in humans. The serotonin transporter protein is involved in the reuptake of serotonin from the synapse, and is critical to serotonin regulation in the brain.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968319/
Serotonin gets downregulated at the genetic level and exhausted from constant stress/inflammation.
Early trauma, immune, and GABA/glutamate
GABA gets downregulated (key to anxiety and neuronal damage).
Long-lasting effects of early-life stress on glutamatergic/GABAergic circuitry in the rat hippocampus
https://pubmed.ncbi.nlm.nih.gov/22245561/
The hippocampus is a key site for mood management and it's very vulnerable to stress and infection. It's also a major site of neurogenesis (brain repair/change).
Early trauma, immune, and anandamide
The endocannabinoid system is tasked with balancing the immune system and anandamide is its key "calming" agent.
Many of the mental health issues show heightened anandamide (i.e. levels in the spinal cord with schizophrenia).
This is essentially the body working overtime to try and right the ship and early trauma can set this stage…
We're finally getting research to show this connection!
Exposure to MS resulted in bidirectional changes in AEA and 2-AG tissue levels within the amygdala and hippocampus and produced a sustained reduction in eCB function in the hippocampus at adulthood. CB1 receptor densities across all brain regions were generally found to be downregulated later in life following exposure to MS.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6347425/
MS is short for maternal separation...a testable type of early stress for the animal
Essentially, early stress reduced anandamide function later in life. Check out our review on endocannabinoid deficiency.
Or this…
The PTSD group also had lower levels of the neurotransmitter anandamide, an endocannabinoid that binds to CB1.
https://www.sciencedaily.com/releases/2013/05/130514085016.htm
Again, stress and trauma, even early, can cause our balancing system to slow down.
Let's turn to general inflammation in the brain.
Early trauma, immune, and brain inflammation
We'll start with the microglia since they govern brain inflammation states.
We found that the number and motility of filopodia-like protrusions of microglial processes tended to increase in the SSC of early-life stressed mice.
https://link.springer.com/content/pdf/10.1007/s12576-015-0361-z.pdf
Essentially, early life stress caused microglia to be more active.
There's a monster review of all the various pathways and elements at this review but we can't put it better than this:
Altogether, early-life stress tends to have a programming effect on neuroimmune functions, mainly resulting in an immediate immunosuppressive, but pro-inflammatory state in adulthood, which triggers an exaggerated neuroimmune response defined by cytokine secretion and microglia activity upon an immune challenge.
https://www.frontiersin.org/articles/10.3389/fnmol.2014.00103/full
We need to unwind this! More on that below.
Let's look at how this translates into risk for specific mental health issues.
Early trauma, immune, and anxiety
It turns out that early life stress affects how our stress response systems will react throughout our life.
It's a thermostat setting of sorts.
We've seen various brain areas thrown about above. Anxiety involves the intersection of three critical players:
- Amygdala - fear and emotional processing center; too much activity can lead to anxiety
- Pre-frontal cortex - rational constraint on the amygdala; too little activity can lead to anxiety
- Hippocampus - powerful mood manager
You see the results of early life stress and trauma all over these areas as it pertains to anxiety.
For example:
Non-human primates, subjected to ELS (variable foraging demand), demonstrated an increase in amygdala volume as assessed by MRI. This increase of amygdala volume was correlated with elevated CSF CRF concentrations, along with reduced hippocampal neurogenesis and increased anxiety
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5482282/
Essentially, an increase in the actual volume of the amygdala and a reduction in the hippocampus following early life stress.
We're talking about the very circuit of anxiety (see Pathways of Anxiety).
Early life stress also shapes our stress response system (called the HPA axis).
The result of this:
In addition to melancholic depression, a spectrum of other conditions may be associated with increased and prolonged activation of the HPA axis, including panic, GAD, phobias and anxiety.
https://link.springer.com/chapter/10.1007/978-981-32-9705-0_9
A who's who of the anxiety spectrum players.
Notice the note on depression at the beginning there?
Early trauma, immune, and depression
Let's start with the mic drop:
Childhood stress and trauma predispose individuals for increased inflammatory tone and major depression in later life, suggesting that early life reprogramming of the stress/immune axis may be involved in the pathogenesis of depression.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898393/
Stress and immune axis. The endocannabinoid system balances both.
Now, why do some people have early stress/trauma and not show signs later in life?
This is the genetic piece. For example, if serotonin is downregulated by early trauma/stress, and you have a variant of serotonin transporter genes that run slow, this can be a major issue.
Or maybe you make lots of estrogen and/or testosterone to support serotonin...in which case you might not be hit as hard.
Resilience can come from genetic differences across multiple pathways.
This is a powerful statement on the effects via the immune system:
Our data suggest a linear relationship between childhood sexual abuse and increased pro-inflammatory cytokine levels in MDD patients, while more recent stressful life events were not related to these inflammatory markers.
https://pubmed.ncbi.nlm.nih.gov/27448525/
See why we're so curious about early trauma/infection? The earlier the trauma, the more likely to cause issues later in life!
What about developmental diseases?
Early trauma, immune, and schizophrenia
Viral infection, especially during critical periods of brain development appear to be suspect:
Separate meta-analysis involving 1035 cases and over 1.2 million controls suggested all childhood CNS infections, particularly viral infections, may be associated with nearly two-fold risk of adult schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3485564/
Other bacterial infections such as toxoplasmosis (from cat feces) are also suspect:
In one study of 63 individuals, who developed schizophrenia spectrum disorders, maternal sera obtained during pregnancy showed an increased risk (OR 2.61) of having IgG antibodies to T. gondii.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2526131/
The key here is this...the immune system not only fights infections but manages the architecture of the nervous system and brain!
We see similar risks with autism, bipolar, ADHD, and the bulwark of developmental diseases.
Early trauma, immune, and dementia
How could stress when you're a child affect old age brain deterioration like dementia?
The immune system!
Childhood stress was associated with increased risk of dementia (HR = 1.86, 95% CI: 1.12–3.10). Associations remained statistically significant after adjustment for age, education, income and other covariates (HR = 1.93, 95% CI: 1.14–3.25)
https://academic.oup.com/eurpub/article/28/6/1069/5055415
More sophisticated studies are unpacking the epigenetic connections...how our experience turns DNA on and off.
A range of genes are at play with many dealing with immune response and inflammation. In fact…
In epidemiology, effect sizes for direct concurrent links in humans are modest, and have best supported inflammatory causations, also by inclusion of other diseases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6194433/
"Best supported inflammatory causations". Immune system people.
One final note.
Early infection and PANDA
There is literally a whole umbrella of OCD that can be triggered by strep infection in kids.
What is PANDA?
Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS) is the sudden, rapid-onset of obsessive compulsive behavior, as well as possible movement and behavioral abnormalities, following a Streptococcus pyogenes (Group A Strep) infection.
https://kids.iocdf.org/professionals/md/pandas/
An infection that directly leads to a mental health issue.
There's fascinating new research that points to the gut as a major player in this and inflammatory ties to mental health in general.
Let's go there!
The gut and brain blood barrier
It's called our second brain. The gut. Mainly because it's the only place outside of the skull that you have such a large network of neurons.
The enteric nervous system as it's called.
Most of your serotonin is actually made in the gut and some is actually synthesized by the countless bacteria that reside there.
The gut inflammatory state (essentially, what level of defcon is the immune system on) acts as a thermostat for systemwide immune response.
This makes sense since it's the first intercept for foreign pathogens that hitchhike with our food.
The gut barrier quite literally is the separation between our most vulnerable inner selves and the hostile outside world.
There's also a barrier that protects the brain as well.
Remember how strep can cause OCD suddenly in children?
Researchers now know why:
Researchers have discovered how immune cells triggered by recurrent Strep A infections enter the brain, causing inflammation that may lead to autoimmune neuropsychiatric disorders in children.
https://www.cuimc.columbia.edu/news/how-recurrent-strep-infections-affect-brain
If the gut and/or brain barrier is disrupted (see our big reviews on gut barrier), pathogens can cross over and cause an immune response in the brain.
There's also the question of the inflammatory state of the gut itself.
Every mental health issue has some correlation with gut inflammation including the two most common:
Dysbiosis and inflammation of the gut have been linked to causing several mental illnesses including anxiety and depression, which are prevalent in society today.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
Let's turn to the newest kid on the research block. The gut-brain axis.
The gut-brain axis via the vagus nerve
The gut and brain barriers are powerful barriers to entry but it turns out the brain and gut have a direct line to each other.
The red telephone if you will.
To wrap it up in a bow:
The autonomic nervous system, hypothalamic-pituitary-adrenal (HPA) axis, and nerves within the gastrointestinal (GI) tract, all link the gut and the brain, allowing the brain to influence intestinal activities, including activity of functional immune effector cells; and the gut to influence mood, cognition, and mental health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
This is fascinating!
Keep in mind that the bacteria in our gut directly manage neurotransmitters in the brain.
Researchers used to think that anxiety, depression, and mood disorders were just a response to gut diseases but the tie is more direct:
The ENS may trigger big emotional shifts experienced by people coping with irritable bowel syndrome (IBS) and functional bowel problems such as constipation, diarrhea, bloating, pain, and stomach upset.
https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-brain-gut-connection
The ENS stands for enteric nervous system...the gut's neuronal web.
How do these two systems communicate?
A big part of it comes from the vagus nerve. The immune system state in the body
There is preliminary evidence that vagus nerve stimulation is a promising add-on treatment for treatment-refractory depression, posttraumatic stress disorder, and inflammatory bowel disease. Treatments that target the vagus nerve increase the vagal tone and inhibit cytokine production.
https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00044/full
So...stimulating this nerve right behind your breastplate reduces inflammation! Cytokines!
That's singing, humming, chanting, tapping, and the new torso twisting that's all the rage on TikTok.
We have a huge review on supporting the vagus nerve which is key to recovering from...viral infections!
To drill further into this...inflammation in the gut can trigger inflammation in the brain!
Stimuli in the intestine can trigger vagal afferent signaling, which is a critical component of neuroimmune inflammatory reflex circuits that contribute to tonic peripheral immune regulation
https://www.nature.com/articles/s41531-016-0002-0
The general "state" of inflammation goes up.
Check out gut barrier inflammation and probiotics for anxiety as examples.
One more stop (we promise).
Oxidative stress and mental health
Oxygen is a byproduct of energy production and the brain is heavily energy-consuming.
Oxygen byproducts (called oxidants...as in anti-oxidants) are like little chemical scissors...they cut through anything and everything including neurons, synapsis, and vital brain architecture.
Here's the connection with immune system function:
Chronic inflammation is characterized by longstanding microglial activation followed by sustained release of inflammatory mediators, which aid in enhanced nitrosative and oxidative stress.
https://pubmed.ncbi.nlm.nih.gov/26831258/
Enhanced oxidative stress. Not good.
Here's the rub...remember that microglia oversee brain growth, repair, and removal.
The way our body gets rid of faulty or damaged cells is with oxidative stress.
It overwhelms the cells and triggers other pathways to come and clear the debris (called autophagy).
In fact, chemo or radiation treatments for cancer are just massive doses of oxidative stress.
In the presence of inflammation and the damage it causes, surrounding microglia call in death squads:
Protein aggregation and neuronal damage result in the activation of disease-associated microglia (DAM) via damage-associated molecular patterns (DAMPs). DAM facilitate persistent inflammation and reactive oxygen species (ROS) generation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7463655/
To summarize..signs of damage trigger the microglia to release oxidative stress.
This is key to neurodevelopmental disorders like dementia, Parkinson's, and autism as well.
Check out our review on oxidative stress here.
We have powerful pathways to keep oxidative stress under control since it's so destructive in the brain.
This finally brings us to the most important section...how to support all these pathways and possible bring the immune system back in balance.
Tools to calm brain inflammation for mental health
Okay...hopefully, this is the payoff for all this work above.
Interestingly, there's a significant crossover between tools for immune function and mental health.
Go figure.
Here are the key tools we'll look at based on safety:
- Vitamin D
- Berberine
- Magnesium Glycinate
- Steroidal hormones
- CBD isolate
- NAC
- Mushrooms (both magic and ordinary)
Let's get started!
Vitamin D
Vitamin D is a master regulator of immune function. Turns out that roughly half the population is deficient and that's based on the ridiculous 30 ng/ml level for bendy knees and Ricketts!
In addition, animal and laboratory studies suggest vitamin D protects neurons and reduces inflammation.
https://www.scientificamerican.com/article/does-d-make-a-difference/
And the microglia hyperactivation?
Neuron-Specific Vitamin D Signaling Attenuates Microglia Activation and CNS Autoimmunity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7005247/
Endocrinologists want us over 60-70 and new studies on that which shall not be named say levels over 50 are incredibly protective.
The ties with mental health and sleep from adequate D levels are equally powerful.
Just look at the tie between sunlight exposure, winter, and depression. SAD...Seasonal Affective Disorder.
Check out our full review of D. Get your levels tested!
I have a version of the VDR gene where I don't process D well. I have to take 10K daily just to get it to budge. Test and adjust accordingly.
Let's turn to the gut.
Berberine
Berberine is a fascinating natural alternative to metformin which has known effects on metabolic pathways, longevity...and gut barrier/inflammation.
Remember, the gut drives the brain's inflammatory state so righting that ship comes first.
First...mental health:
Berberine, a natural isoquinoline alkaloid, is used in herbal medicine and has recently been shown to have efficacy in the treatment of mood disorders. Furthermore, berberine modulates neurotransmitters and their receptor systems within the central nervous system.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6307759/
What about the immune system in the brain?
Our findings also demonstrate that berberine significantly down-regulates LPS- or interferon (IFN)-gamma-induced nitric oxide synthase (iNOS) and cyclo-oxygenase-2 (COX-2) expression in BV-2 microglia cells. Berberine also inhibited LPS- or IFN-gamma-induced nitric oxide production.
https://pubmed.ncbi.nlm.nih.gov/20512929/
Goodness...that's a hodgepodge of inflammatory and oxidative stress agents in the brain.
Check out our review of berberine.
Next up, a key mineral player.
Magnesium Glycinate
Mag is amazing and so many people are deficient.
Our food doesn't have it any longer since our soil has been destroyed from mono-crop and pesticides.
The bacteria in the soil is what transfers minerals and nutrients to our food!
Enough preaching.
We've covered mag's effect on mental health and sleep extensively here.
What about the immune system?
Look at the effects after mag deficiency:
The characteristic allergy-like crisis of Mg-deficient rats was accompanied by a blood leukocyte response and changes in leukocytes subpopulations. A significant increase in interleukin-6 (IL-6) plasma level was observed in Mg-deficient rats compared to rats fed a control diet.
https://www.sciencedirect.com/science/article/pii/S0925443900000181
Deplete mag and the immune system hyperactivates! Histamine response (the source of allergies) is a key part of the immune system and it gives away the clue...an allergy explosion.
Check out our allergy response. Keep in mind that histamine is critical for insomnia (more on that here).
Here's the mental health piece beyond brain inflammation.
Mag directly supports GABA, our brain's brake pedal. This is critical for anxiety, depression, and the suite of mental health issues.
It's also your primary sleep support. See our sleep review.
We have a major magnesium glycinate review here.
Glycinate crosses the blood/brain barrier best. You can take up until you have diarrhea (it's a laxative).
Let's get to the heart of the issue (in our mind).
Steroidal hormones
So many age-related issues are the result of steroidal hormones going down.
Progesterone is a huge player in calming the immune system. Estrogen directly supports it. The two work together to manage our immune response with huge implications for mental health.
Here's the deal...progesterone drops by 50% at age 40 and continues down. Estrogen plummets around late '40s during perimenopause.
A brutal perimenopause is actually what started us down this journey (that story is here).
Estrogen directly supports serotonin and progesterone directly supports GABA. Two of the most powerful neurotransmitters in the brain!
Anxiety. Depression. Mood disorders. You name it...they're involved.
Testosterone functions much like estrogen for men and it drops 1% each year from about age 20. In the male brain, it gets turned into estrogen for the neuroprotective and growth brain pathways.
Check out reviews on progesterone, estrogen for mental health, and testosterone to learn more.
Also, we looked at whether decreasing steroidal hormones are the key to aging.
Next up...close to our heart.
CBD Isolate
Hopefully, you can tell...we love research! Real research...NIH studies, etc.
The more we dove into CBD, the more intrigued we became.
CBD supports the endocannabinoid system (remember anandamide???) when running low.
It works like a feedback mechanism in that it doesn't push in one direction.
This is critical since we don't want tolerance.
Its cousin, THC, pushes in one direction on CB1 receptors and therefore, it builds tolerance with time and has other "overreach" side effects.
CBD does not.
One example (of 100's) that is powerful with the immune system and oxidative stress.
- Healthy cell or neuron with low inflammation - CBD has no effect
- Healthy cell or neuron with high inflammation - CBD reduces inflammation
- Cancerous or virally infected cell/neuron - CBD INCREASES inflammation
Three different results depending on the state of the cell.
Why the third response? Remember that the immune system (under guidance from the microglia) will jack up oxidative stress to kill off cells.
CBD is supporting this natural process without affecting neighboring healthy cells!
CBD supports serotonin, GABA, stress response, and more.
Two quick takeaways:
cannabidiol (CBD) has emerged as a promising strategy to treat inflammation that results from microglial hyperactivation [78], with no psychotropic side effects. Moreover, CBD has been shown to attenuate oxidative and nitrosative stress in several human disease models
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3386505/
Okay…
- Hyperactive microglia. Check.
- Not psychoactive. Check.
- Reduce oxidative stress. Check.
We could go and on but check our CBD and neuroinflammation for anxiety review.
As for mental health, we have a massive review of CBD and mental health here with breakout deep dives for all major illnesses.
Next up...our second favorite behind CBD.
NAC
NAC is a powerful tool against excessive glutamate (remember, toxic when too high) and also calming oxidative stress.
We have a massive NAC review on the mental health benefits but what about the immune system?
A fascinating study looked at how microglia become hyperactivated (sound familiar) following antiviral drug cocktails for HIV:
We demonstrated that exposure of microglia to the chosen cART cocktail induced generation of reactive oxygen species, subsequently leading to lysosomal dysfunction and dysregulated autophagy, ultimately resulting in the activation of microglia. Intriguingly, the potent antioxidant, N-acetylcysteine, reversed the damaging effects of cART.
https://www.frontiersin.org/articles/10.3389/fneur.2020.00840/full
Finally, another study looked at how social defeat (animal study term for psychological stress) triggered microglia which lead to the animal version of depression and self-isolation.
NAC's impact:
NAC during microglial recovery prevented the belated decline in social investigation seen during repopulation. It also elevated time investigating social targets in previously CSD-stressed mice that did not have microglial depletion.
https://www.jneurosci.org/content/39/28/5594/tab-figures-data
Most importantly, the study found that this result was from blocking oxidative stress (inflammation!!).
Finally, mushrooms.
Mushrooms
We already did a full review of psilocybin for mental health here. It's going to revolutionize the space over the next 5 years.
If you're not ready for that yet, take a look at their more common cousins.
Turkey Tail (review here) is a powerful player with cancer pathways...primarily fine-tuning the immune system to seek out and destroy cancerous cells.
Remember, the immune system is in charge of cellular birth/death cycles.
Even standard mushrooms directly interact with the immune system in a positive way.
Here's your guide to medicinal mushrooms and the immune system with an emphasis on mental health.
But just a teaser:
It is well-established that mushrooms are adept at immune modulation and affect hematopoietic stem cells, lymphocytes, macrophages, T cells, dendritic cells (DCs), and natural killer (NK) cells.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4684115/
Remember, the long-term effects of psilocybin were narrowed down to triggering DNA tied to immune function!
We'll wrap with that. It's an exciting new world of discovery. Check out the Inflamed Mind by Edward Bullward. A fascinating introduction.
Be well. Take care of each other. Take care of yourself!
Related Research:
Psilocybin Guide
Early trauma/infection and mental health
Guide to building resilience
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.