Guide to CBD's Effects for Schizophrenia and Psychosis

This is personal for us.
I have a brother who is diagnosed with paranoid schizophrenia.
He had been living on the streets for about a decade now and only recently come into shelter.
It's a heartbreaking few decades with my parents baring most of it.
He just recently (age 39) agreed to have a cell phone which was a major breakthrough.
I was put on the phone with him and although his voice sounded much better, he didn't believe it was me.
It was shocking to hear such a lucid and seemingly upbeat voice (much improved since years ago) combined with the paranoia bent.
The two seemed diametrically opposed.
I've been dreading writing this review, not because of the heartbreaking nature of the disease but because this is going to be involved.
If we're going to do it right. Based on NIH research. All the known and current facets.
There are pretty amazing tools out there now which research is showing can have an impact on the disease.
CBD is front and center (the initial study was nothing short of amazing).
New insight is pointing to the immune system's role and we have powerful tools there as well.
It's a glimmer of hope until we unravel the disease further.
We'll cover these topics:
- What causes schizophrenia based on current research
- Early infection or trauma and schizophrenia
- Genetics and schizophrenia
- Brain areas and schizophrenia
- Neurotransmitters and schizophrenia
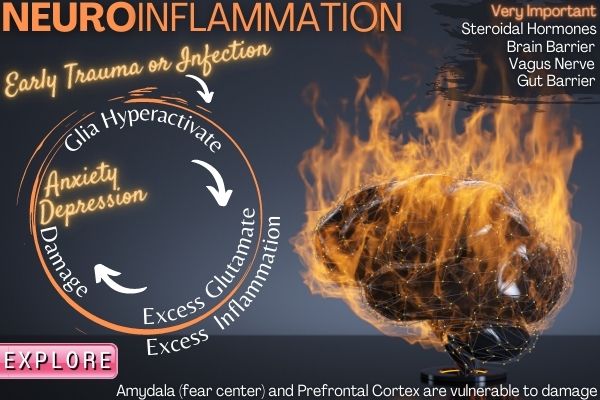
- Inflammation and schizophrenia
- Immune response, microglia, and schizophrenia
- The opioid system and schizophrenia
- The gut microbiome and schizophrenia
- Early infection and schizophrenia
- THC and schizophrenia
- Can CBD help with schizophrenia
- Other promising tools for schizophrenia
- CBD versus antipsychotics for schizophrenia
- CBD for paranoia
- How much CBD to take for schizophrenia
- What's the best kind of CBD for schizophrenia
Like we said...this is personal for us and if you've looked at any of our other reviews, we go deep.
Periscope down.
What causes schizophrenia based on current research
There is an outstanding look at common questions for schizophrenia (including early warning signs) here:
https://www.helpguide.org/articles/mental-disorders/schizophrenia-signs-and-symptoms.htm
As you scroll down, take a look at the role of certain stressors during critical periods of brain development:
- Prenatal exposure to a viral infection
- Low oxygen levels during birth (from prolonged labor or premature birth)
- Exposure to a virus during infancy
- Early parental loss or separation
- Physical or sexual abuse in childhood
They center around infection, stress, and trauma!
That's our first big clue and we'll drill way down into this as we go further.
We'll look at the genetics below but it's estimated that 60% of people diagnosed with schizophrenia have no family members with the disease.
There are intriguing clues across inflammatory and immune pathways that are coming out all the time now.
More importantly, there are ways to calm those pathways and we'll touch on those below.
Before we drill down further, the current theory from a top-down view:
- Genetic susceptibility affects reactions to stress
- A stressor is introduced at critical periods of brain development
- The immune system overreacts and over-prunes the brain architecture
This is not too far from the basis for all auto-immune diseases (see CBD and neuroinflammation).
Instead of joints (arthritis) or islet cells (Diabetes), it's brain architecture.
That's the big picture based on current research.
Granted, it's a simplification for a very complicated disease but when you see the study on CBD and schizophrenia, maybe not so much.
Let's break it out now and shed light on why this thought is emerging.
Genetics and schizophrenia
We'll start at the start.
Genetics!
First, there isn't a schizophrenia gene. It's much more complicated than that.
There is definitely a genetic input for "risk" or susceptibility:
A meta-analysis (Sullivan et al., 2003) of twin studies estimates the genetic liability to schizophrenia at 81% (95% CI, 73%–90%), whereas shared environmental influences were estimated to be 11% (95% CI, 3%–19%).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5480258/
Follow up studies showed that adopted children from mothers with schizophrenia had the same risk as their mother but were not affected if the adopted mother was diagnosed.
Here's the interesting part which shows the effect of the environment:
A Finish adoption study (Tienari et al., 1985, 2004) found that markedly dysfunctional rearing environments (the adoptive families were initially assessed and classified on a scale ranging from “1. healthy” to “5. severely disturbed”) predicted schizophrenia spectrum disorders in adopted-away children of mothers with schizophrenia but not in their genetically undisposed controls.
This means that a really bad environment could trigger schizophrenia in a child whose mother was schizophrenic but not in a child without such a mother.
This speaks to stress response and of course, that's partially rooted in genetics.
As for specific genes, it's not that simple.
We can think of schizophrenia as a catch-all disease for many important genes that might be faulty.
For example, even the big one tied to it directly (SETD1a) only shows in 1 out of 1000 people diagnosed with schizophrenia.
The sheer complexity of our nervous system and the underlying machinery paints a more nuanced genetic landscape for schizophrenia.
Some of the most cited candidate genes are DISC1, DTNBP1, NRG1, and COMT, but their potential pathogenetic involvement in schizophrenia remains debated.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5480258/
The more fruitful approach appears to look at stress response genes and schizophrenia.
As researchers put it:
Many studies have demonstrated that genotype (G) interacts with adverse life experiences (E) to produce individual differences in vulnerability and resilience to mental disorders, including schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4332957/
This fits in with the triggers we saw above from England's Health System review.
Trauma. Stress. Infection.
Basically, our body's inflammation response system.
Wait till you see how the endocannabinoid system (where CBD interacts) plays into this.
One interesting genetic player in this whole process deals with dopamine in response to stress.
We'll cover it in the neurotransmitter area but a quick teaser:
Included among the many genes associated with the risk of schizophrenia, are the gene encoding the DRD2 receptor and those involved in the upstream regulation of dopaminergic synthesis, through glutamatergic and gamma-aminobutyric acid (GABA)-ergic pathways.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5675052/
And the clincher...
A number of these pathways are also linked to the stress response.
There's are big hitters such as COMT and MAO of course.
Interestingly, there's a tie between a COMT genetic version and exposure to herpes 1 and 2 viruses (next topic).
Before we get to the manifestations of schizophrenia in the brain, let's circle back to the triggers in more detail.
Early infection or trauma and schizophrenia
This may seem odd or even frightening that schizophrenia can result from the whims of a virus or bacteria.
Unfortunately, there's a great deal of research backing this up.
First, there's the odd distribution of birth months and influenza virus exposure which has been reflected in many studies.
We've known this for a while in fact.
Back when syphilis was unconquered:
Among bacteria, the fact that the spirochete of syphilis can cause the symptoms of schizophrenia was well known to psychiatric clinicians of an earlier era.
Then you have the wonderful cat litter effect with T gondii (toxoplasmosis).
A study looked at the presence of antibodies to T gondii (meaning exposure earlier) in people with schizophrenia:
An overall analysis of the studies indicates that serologic evidence of Toxoplasma infection is almost 3 times more common in persons with schizophrenia than in controls living in the same geographic region
Then there's herpes 1 and 2.
They were tied to the severity of symptoms in people with schizophrenia.
Comparison studies of persons with and without schizophrenia or bipolar disorder show that HSV-1 infection significantly increases cognitive dysfunction—especially recent memory deficits—in persons with schizophrenia or bipolar disorder
Remember how we mentioned the COMT gene and herpes exposure?
What does the COMT gene do?
Oh...it just breaks down stress response hormones. That's all.
What about the study where an anti-viral agent was given to people who had exposure to another known trigger, cytomegalovirus, with persistent schizophrenia:
There was a significant improvement in the psychiatric symptoms of individuals who were seropositive for cytomegalovirus.
https://www.ncbi.nlm.nih.gov/pubmed/14638597
By the way, we all have this in our body as you never lose it and everyone's exposed.
The difference is in the immune response to it!
The timing of exposure to infection can be critical.
Early childhood or even in utero are key points:
A separate meta-analysis involving 1035 cases and over 1.2 million controls suggested all childhood CNS infections, particularly viral infections, may be associated with a nearly two-fold risk of adult schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3485564/
That's a massive review of many studies.
It's not just schizophrenia of course.
Pick your mental health and watch the immune overreaction tie-in with new research.
PANDA's and OCD. Anxiety and depression. Autism, OCD, and ADHD share similar risk factors.
The new field of immunopyschiatry may be the key to all of this!
Check out our CBD and the mechanisms of anxiety as an example of what research is showing.
Here's the rub...the immune system is a one-trick pony (albeit with 100's of different breeds of pony).
It responds similarly to trauma or social stress as to infection!
Observational human studies and experimental animal models suggest that childhood exposure to stress can trigger an enduring systemic inflammatory response, not unlike the bodily response to physical injury.
https://www.annualreviews.org/doi/abs/10.1146/annurev-psych-010416-044208?journalCode=psych
The newer research is fascinating in that it actually points to the opioid system as the connection between early trauma and later mental illness.
We'll get into that below of course.
So...genetic susceptibility combined with trauma or infection during key points of brain development all intersect in one area.
Inflammatory pathways.
We'll look at each section below.
Let's cover the effects of this imbalance across two topics: brain areas and neurotransmitters.
Brain areas first.
Brain areas and schizophrenia
Let's start with brain scans to see what they show.
One study looked at 14 years olds to see if there was a difference in gray matter in the brain:
It found that the teens who had symptoms lost more brain tissue over a 5-year period than the others.
https://www.webmd.com/schizophrenia/schizophrenia-and-your-brain#2
Gray matter can be thought of as the communication interchange between different brain areas.
The connection between early stress and trauma?
More personal early-life stressful events were associated with larger developmental reductions in GMV over anterior prefrontal cortex, amygdala, and other subcortical regions.
https://www.nature.com/articles/s41598-018-27439-5
Interestingly, the biggest impact of this effect shows in two diseases that showed shared pathways among the many mental health illnesses:
Lack of grey matter in the brain is linked to schizophrenia and bipolar disorder.
https://www.sciencedaily.com/releases/2009/01/090116073803.htm
Keep in mind that brain growth and repair is just as critical as the destruction of stress, immune response, and trauma.
That's the other side of the coin.
The focus there is on BDNF and neurotrophins. BDNF is like fertilizer in our brain (check out CBD and BDNF).
Meta-analyses have demonstrated that serum BDNF levels were tightly correlated with the courses of severe schizophrenia and major depression disorders.
Wait till you see what we can do for BDNF below.
Where we're losing this gray matter is very important.
People with schizophrenia have up to 25% less volume of gray matter in their brains, especially in the temporal and frontal lobes.
https://www.gulfbend.org/poc/view_doc.php?type=doc&id=8812&cn=7
The prefrontal cortex, the part of the brain that makes humans human.
This is the rational, organizing area of the brain.
We covered it quite a bit in our CBD for anxiety article since it's intimately tied to the anxiety circuit (countering the amygdala emotional and fear response area).
Here's the interesting piece.
Studies at Yale on early or onset of schizophrenia shows too much activity in the prefrontal cortex:
Compared to people with no history of mental illness, the early-course schizophrenia patients showed a general pattern of increased connectivity unique to medial regions of the PFC.
The antipsychotic medications were shown to reduce this activity a year later.
This goes directly counter to studies of long term sufferers with schizophrenia which show reduced connectivity.
We'll look at the fascinating microglia (part of our brain's immune system) which governs the architecture of our brain to see what might be causing this poor management.
The other area that comes up is the right dorsolateral prefrontal cortex which shows a pattern of reduced activity in people with schizophrenia.
This connection isn't surprising when you understand that the RDPC controls how we respond to outside stimulus:
An important function of the DLPFC is the executive functions, such as working memory, cognitive flexibility,[8] planning, inhibition, and abstract reasoning.
https://en.wikipedia.org/wiki/Dorsolateral_prefrontal_cortex
Of course, you'll see differences across many brain areas that matches what you would expect from a systemic immune or inflammatory response.
The hippocampus is especially vulnerable to stress damage since it's so dynamic (the seat of memory).
The connection between schizophrenia and this area?
The decreased brain volume in schizophrenia is especially pronounced in cortical areas, as well as in the hippocampus.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518924/
Let's drill down a bit further to the actual messengers of the brain.
Neurotransmitters and schizophrenia
There are a few suspects to look at for serotonin but understand that the brain's chemical messaging system is a complicated, interwoven symphony that's constantly in flux!
The key players are:
- Dopamine - the heart of our motivation - excitatory in nature
- Glutamate - our primary excitatory agent in the brain (as opposed to GABA) tied to NDMA pathway
- Serotonin - as a master regulatory, serotonin exhaustion may be key to schizophrenia
Those are some pretty heavy hitters in the brain landscape.
Sure, you can probably find a connection with almost any pathway with a disease as complicated as schizophrenia but these three stands out in research.
They may just be knock-on effects from up-river effects (inflammatory process, immune response, etc) but let's look closer at each.
Dopamine and Schizophrenia
The dopamine theory of schizophrenia basically comes from the effect of antipsychotic drugs that target dopamine processing.
A large number of these medications basically block dopamine signaling, especially at one receptor called DR4.
We're never content to stop there. When we looked further at what is known about the DR4, it's fascinating.
First, genetic versions of it are tied to everything from ADHD, gambling, addiction, and risk-taking (among others).
Further down, there's an interesting section on its control over stress response..., especially during early life.
The DRD4 genotype also moderates the association of experienced parental problems during childhood (e.g., parental depression, marital discord) with loss or trauma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3560519/
It basically controls how early stress and trauma "marbleized" in our personality.
When combined with serotonin gene variants, another effect:
Armbruster et al. [60] found that carriers of the 7R allele together with the 5HTTLPR L allele exhibit lower cortisol stress responses.
This explains the risk-taking and even addiction.
People with a version of this gene may not feel much and are desperately trying to override that DR4 dampening effect.
Just look at the effects on personality for the R7 gene variant:
Results suggest that the long allele (7 and more repetitions) is associated with high novelty seeking and risk-taking, constricted emotional responses, but is also associated with preserved attention processing of emotional stimuli and efficient problem-solving.
Very fascinating.
As for schizophrenia…
In fact, elevated levels of D4 receptor binding have been found post-autopsy in the brains of persons who had schizophrenia.
https://www.scientificamerican.com/article/what-happens-to-the-body/
After our extensive review of CBD and anxiety mechanisms, we recognize a pattern.
The brain (and body) attempt to compensate for deficiencies by boosting other pathways.
Perhaps D4's effect on neutralizing trauma and stress' effect is boosted but comes at a price.
There's a full review of dopamine's association with schizophrenia but the net-net is this:
The “revised dopamine hypothesis” proposes hyperactive dopamine transmission in the mesolimbic areas and hypoactive dopamine transmission in the prefrontal cortex in schizophrenia patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4032934/
This speaks to both the negative symptoms (lack of focus, interest, etc) and the positive symptoms (hallucinations, delusions, etc).
Next up…
Glutamate and NMDA with Schizophrenia
Glutamate is the gas pedal of our brain. It's our primary excitatory messenger.
Keep in mind that this means cellular activity as well.
NMDA is a primary receptor for glutamate which gets turned "on" by its interaction.
Think of NMDA as the gardener of the brain. One of its roles is to determine which way the brain is going to go based on outside experience and genetic constraints.
It's intimately involved in guiding the "plasticity" or change in brain structure.
Sounds relevant to everything we've discussed above (brain area loss, etc)?
The net effect of this guiding hand is "learning" both in terms of algebra and cocaine.
Ca2+ flux through NMDARs is thought to be critical in synaptic plasticity, a cellular mechanism for learning and memory.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518924/
When they looked at vast swafts of genetic profiles to find genes tied to schizophrenia risk, indeed, some NMDA and by proxy, glutamate signals popped up:
As a whole, these recent large-scale studies have identified both common and rare genetic variants in the N-methyl-D-aspartate receptor (NMDAR) genes, as well as components of the postsynaptic density, with increased risk for schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518924/
"Postsynaptic density". Ahhhh….basically, how robust our brain's little branches and root systems are.
Intimately tied to the progression and symptoms of schizophrenia.
Too little activity in this pathway is looking to be the issue:
There is substantial pharmacologic, genetic, and biochemical evidence to support NMDAR hypofunction as a key etiological component of schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518924/
In fact, we can look to lovely PCP (an NMDA blocker) which elicits many schizophrenia symptoms in healthy subjects.
We'll end this section with a very cleverly crafted study.
Researchers used low dose PCP to create schizophrenia-like symptoms in mice.
For half the mice, they administered the influenza virus at a key point in development (way before PCP administration).
Here's the fascinating result:
Virus-infected mice tended to be more susceptible to these PCP-induced deficits in cognition and showed a clear difference in motor activity when compared to the control mice.
https://pdfs.semanticscholar.org/87d9/79cc8474c7169225cd1dd41ba22e80321fdd.pdf
They then go on to pinpoint changes in NMDA activity from this effect.
There are instances where the body's immune response attacks the NMDA system (NMDAR antibodies and encephalitis).
We would need another full review to look at the immune system "modeling" from early infection/trauma and NDMA function but here's a clear point:
Using a combination of single molecule-based imaging approaches, we here ascertain the presence of circulating autoantibodies against glutamate NMDA receptor (NMDAR-Ab) in about 20% of psychotic patients diagnosed with schizophrenia and very few healthy subjects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5702610/
The studies above clearly point in a direction. Too much glutamate activity to in the beginning and the body pushing back to reduce glutamate function.
We'll look at Glycine's role and potential in this pathway below in our tools for the schizophrenia section.
Finally, serotonin.
Serotonin and schizophrenia
Serotonin is a master messenger in the body and gut.
We would expect it to be implicated or at least affected by schizophrenia.
What do researchers say:
Chronic widespread stress-induced serotonergic overdrive in the cerebral cortex in schizophrenia, especially in the anterior cingulate cortex (ACC) and dorsolateral frontal lobe, is the basic cause of the disease.
https://www.ncbi.nlm.nih.gov/pubmed/23557849
Did you catch that first part??
"Stress-induced". This matches the early triggers of trauma and infection.
Also, the ACC (communication tract) and there's the dorsolateral frontal lobe from above.
In this case, it's serotonin overdrive...too much serotonin trying to quell inflammation.
There's a whole class of medications called neuroleptics that block or slow down serotonin transmission.
Their effects?
And the fact that blockade of serotonergic 5-HT2A receptors by atypical neuroleptics slows down the course of the disease.
Serotonin has its fingers in many pies including the dopamine and glutamate (NDMA) pies above.
Watch this effect here:
Disruption of glutamate signaling by serotonergic overdrive leads to neuronal hypometabolism and ultimately synaptic atrophy and grey matter loss according to principles of brain plasticity.
https://www.ncbi.nlm.nih.gov/pubmed/23557849
Is the brain boosting serotonin to quell excess glutamate...caused by hyperactive immune respousne (which just gushes glutamate)?
Remember how we said that schizophrenia shares pathways with bi-polar as opposed to other mental health diseases?
Increased DNA methylation status of the serotonin receptor 5HTR1A gene promoter in schizophrenia and bipolar disorder.
https://www.ncbi.nlm.nih.gov/pubmed/21453976
5HT is serotonin. This statement just means that the brain is overproducing serotonin.
There's an intimate relationship between serotonin and glutamate. In fact, they can operate almost as a collective:
Particularly, it has been demonstrated that serotonin (5-hydroxytryptamine) 2A (5-HT2A) receptors and metabotropic glutamate type 2 (mGlu2) receptors can assemble into a functional heteromeric complex and modulate each other’s function.
Here's the fascinating thing about serotonin:
Psychological stress, wherein emotional factors were predominantly involved, significantly increased extracellular 5-HT levels in these two areas.
https://www.sciencedirect.com/science/article/abs/pii/0304394093905653
We've looked at serotonin in detail at our CBD and serotonin review.
Let's move on to the star player in all of this with fascinating research.
Inflammation and schizophrenia
Think of inflammation as disruption in the nervous system.
Basically, it requires our immune system's response.
This can take the form of infection, stress, and even trauma.
A big part of this stress response is via corticosteroids like cortisol (see CBD and cortisol).
There's an impressive review that looks at the role of corticosteroid release during key periods of brain development.
Some prominent takeaways.
The review goes through dozens of studies that point to early interaction with infection or stress resulting in glucosteroids (stress responders) which affect brain development.
Other sources of stress and inflammation also increase risks such as obesity or starvation.
Here's probably our favorite take away (of many):
The dependence on glucocorticoids has been confirmed by treating pregnant dams with dexamethasone during the final week of gestation which also leads to reprogramming of the set point of the stress axis in the adult offspring.
https://www.nature.com/articles/1395839
Read that again.
Early exposure to corticosteroids affects the "set point" of the stress response.
Think about that for a minute. Why can some people handle more than others? What if your set point is severely reduced from early exposure to stress/infection?
The review then goes on to the effects of a poor stress response.
- Reduced brain volume in the hippocampus
- Dysregulated dopamine and glutamate function
- Increased serotonin levels in certain areas
Goodness...our immune system is "markedup" by past stress and it controls brain archtecture.
What about the telltale signs of inflammation with schizophrenia.
Let's look at:
- Cytokines
- Oxidative stress
- Corticosteroids
First, cytokines and schizophrenia.
Cytokines are the little inflammatory assassins the body creates in response to enemies.
Unfortunately, they can also be triggered by stress and they're known to create a lot of collateral damage.
And with schizophrenia?
Levels of pro-inflammatory markers, such as cytokines, have been found to be increased in the blood and cerebrospinal fluid of patients with schizophrenia.
https://www.ncbi.nlm.nih.gov/pubmed/29648618
Here's the real clincher.
Watch what happens with chronic inflammation on all the pathways we discussed above:
Typical alterations of dopaminergic, serotonergic, noradrenergic, and glutamatergic neurotransmission described in schizophrenia have also been found in low-level neuroinflammation and consequently may be key factors in the generation of schizophrenia symptoms.
As we mentioned above, there's lots of collateral damage...our brain areas and the informational tracts between them.
The hippocampus is especially vulnerable.
We'll look at the microglia (sentries in our immune response) later on but they're critical.
The most fascinating piece that's relatively new centers around inflammation and kynurenic acid which we broke out into a separate section below.
Interestingly, many of the anti-psychotics actually modify inflammatory and immune response!
Check out CBD and inflammation here.
Let's look at oxidative stress.
Oxidative stress and schizophrenia
Our brain uses a tremendous amount of energy.
As a result, it creates an equivalent amount of waste material from this energy production.
It's usually in the form of different forms of oxygen spun off from our power plants, mitochondria.
These "free radicals" are like little scissors running around little bags filled with water (our brain cells) not to mention the DNA inside them.
Not great.
Check out CBD and oxidative stress.
To protect us, we have a robust system to clear out oxidation. Antioxidants. Redox technically.
So...is there a tie between schizophrenia and oxidative stress?
Currently, the available evidence points towards alteration in the activities of enzymatic and nonenzymatic antioxidant systems in schizophrenia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021756/
That makes sense since stress creates oxidative stress.
Even more fascinating is that researchers can ramp up oxidation in healthy subjects and guess the effects:
In fact, experimental models have demonstrated that oxidative stress induces behavioral and molecular anomalies strikingly similar to those observed in schizophrenia.
Oxidative stress is directly linked to the litany of mechanisms we looked at above.
More importantly, a powerful antioxidant approach has been shown to calm symptoms of schizophrenia.
We'll get into the best ones we've found below in our tools for the schizophrenia section.
The big player there is glutathione (see CBD and glutathione).
New studies are finding that the overactive inflammatory response may exhaust glutathione during the initial phase of the disease:
These findings are consistent with the hypothesis that excitotoxicity during the acute phase of illness leads to reduced glutathione and glutamate in the residual phase of the illness.
https://www.nature.com/articles/s41380-018-0104-7
People...this is definitely something we can work on!
Finally…
Corticosteroids and schizophrenia
We mentioned the comprehensive look at early exposure to corticosteroids and brain development risk for schizophrenia.
Corticosteroids are our stress response hormones.
They're incredibly powerful in the body and designed to respond to danger!
It's that shot of cortisol when a car veers at you.
This is life and death stuff so they override most other inputs.
What about after early development? What do we see there?
First, it's known that corticosteroids (the drug) can induce psychosis at higher doses:
In addition, high dosages of prescription corticosteroids (eg, prednisone and dexamethasone) are associated with mood changes, cognitive deficits, and even psychosis.
https://link.springer.com/article/10.1007/s11920-002-0023-8
What our primary corticosteroid...cortisol.
This gets interesting!
The relationship between two chemicals released when people experienced stress—one released in the brain and the other in saliva—differs in people with schizophrenia.
https://medicalxpress.com/news/2018-07-stress-affects-people-schizophrenia-differently.html
The two chemicals?
Dopamine and cortisol!
Their analysis:
"Cortisol is the main stress hormone, so this suggests a disrupted stress regulatory system in people with schizophrenia," says Dr. Mizrahi.
This keeps pointing back to the stress response being faulty.
So...how does the body respond to all this inflammation in the context of schizophrenia?
Immune response, microglia, and schizophrenia
Many clues are pointing to an over-active response as a key pathway of schizophrenia.
The connection with early viral and infection exposure is that the immune response is transferred to the baby from the mother.
Let's look at microglia, shall we!
microglia are immune agents in the brain and nervous system.
Sentries on the look-out for bad actors.
That's not their only role though!
It turns out they directly involved in "landscaping" our brain's architecture.
The tie with schizophrenia?
This excessive synaptic pruning reflects abnormalities in both microglia-like cells and synaptic structures.
https://www.nature.com/articles/s41593-018-0334-7
This partially explains why schizophrenia tends to appear during puberty when the brain goes through an extensive "remodeling" for the adult brain.
This is carried out by the microglia.
People, this is all in the last few years that we finally have research pointing to hyperactivation as a trait of schizophrenia (and many other mental health issues).
Here's the interesting piece...microglia "threat response" can be primed by early infection and trauma:
Microglial “priming” or increased sensitivity to subsequent insults is one of the proposed mechanisms.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5758507/
Think of how you operate when stressed out and over-taxed.
Now imagine your immune system's the same way.
The knock-on effects are powerful once you realize that this system is tasked with cell birth/death in the brain:
Priming could also prevent microglia from exerting their normal physiological functions, directly impairing neurogenesis, synaptogenesis, and the wiring of brain circuits, with severe impacts on learning, memory and other cognitive processes.
- Neurogenesis - making new neurons
- Synaptogenesis - making new connections
Goodness.
This is in addition to the inflammatory response which also suffers when our immune system is "primed" hot by prior experience.
Check out CBD and microglia for neuroinflammation where we really get into it.
Let's look at potential cog in that wheel tying it together.
Kynurenic acid and schizophrenia
You probably haven't heard of this one yet.
This is a metabolite of tryptophan (see CBD and tryptophan for anxiety).
It happens to be neuroactive and generally acts as a "brake" in the nervous system.
This allows it to block excitatory neurotransmitters which can lead to cell death if excessive and even anti-convulsive actions.
A large review of many other studies found this relationship:
Overall, KYNA levels are increased in patients with schizophrenia, specifically within the central nervous system.
https://www.ncbi.nlm.nih.gov/pubmed/28187219
Interest grew when researchers found that by blocking NMDAR activity, they could elicit symptoms in healthy volunteers and in people with schizophrenia.
What's the one known, naturally-occurring in the body NMDA blocker?
Kynurenic acid!
The plot thickens.
Think of kynurenic acid as a check and balance on glutamate (our gas pedal) activity.
Too much glutamate is bad as it will kill cells. The term is cytotoxic.
Think of revving an engine into the red zone for too long.
Here's where it gets interesting:
Preclinical studies manipulating levels of KYNA have demonstrated its influence on both behavior (eg, cognitive functioning) and neurotransmission (eg, glutamatergic, dopaminergic) observed to be aberrant in patients with schizophrenia.
https://academic.oup.com/schizophreniabulletin/article/43/4/764/2982261
Remember how there was a tie between bipolar and schizophrenia?
This kynurenic pathway may be the key.
Genetic studies found a shared gene directly in this pathway:
After replication in an independent cohort, we linked this genetic variant—associated with reduced SNX7 expression—to positive psychotic symptoms and executive function deficits in bipolar disorder.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4965332/
But wait a minute...we've spent the better part of 5000 words looking at effects of stress and inflammation response.
How does it figure in with the kynurenic effect?
The study found elevated kynurenic acid in the brains of people with schizophrenia suggesting an overproduction of kynurenic acid, especially in response to inflammation, which could be detrimental to brain function.
https://medicalxpress.com/news/2019-04-inflammation-linked-chemical-imbalance-schizophrenia.html
"Response to inflammation".
This brings up one of the tools we'll talk about below...glycine.
What is the relationship of kynurenic acid to glycine??:
A competitive antagonist of glycine co-agonist sites of the N-methyl-D-aspartic acid receptor.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4318830/
They both battle for a turn at the NMDA receptor!
Let's give kynurenic a run for its money (more on that below).
The opioid system and schizophrenia
Like we said...no stone left unturned.
You may be thinking that the opioid system is only for pain.
Nothing's that easy in the body.
There are different receptors and one of them (Kappa opioid receptor or KOR) is fascinating.
We studied it in depth in our review of low dose naltrexone and SSRIs and suicidal or homicidal thoughts.
The reason why it's important here:
In contrast to the mu-opioid receptor and delta-opioid receptor agonists, KOR agonists are potent psychotomimetics in healthy people.
https://www.biologicalpsychiatryjournal.com/article/S0006-3223(19)31379-4/pdf
Psychotomimetics - mimics results of psychosis.
Okay...we're listening!
Researchers realized this when they gave patients drugs which increased KOR activity:
It was shown that cyclazocine and ketocyclazocine could induce paranoid delusions and hallucinations of monsters.
https://www.biologicalpsychiatryjournal.com/article/S0006-3223(19)31379-4/pdf
The most important word in that whole sentence is "paranoid".
For anyone with first-hand interaction with the disease, paranoia is by far the worst part of it. Check out CBD and paranoia.
It blocks the ability to get help!
More frustrating is that it's a very intractable, seemingly too complex symptom to address.
Wait till you see CBD effects on paranoia below.
In fact, the effect of THC to induce psychosis may be dependent on this pathway:
Thus, THC in the posterior NASh produces dose-dependent aversion effects that are dependent upon local KOR transmission but independent of MOR transmission.
https://www.nature.com/articles/s41598-019-46215-7
We'll get into THC and schizophrenia below.
Here's why we geek out on this KOR pathway.
Early-Life Social Isolation Stress Increases Kappa Opioid Receptor Responsiveness and Downregulates the Dopamine System.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4946054/
Remember the two last triggers from way up above:
- Early parental loss or separation
- Physical or sexual abuse in childhood
Very interesting. This still falls in our stress/inflammatory response vein.
Let's go south. To the gut!!
The gut microbiome and schizophrenia
All roads lead to the gut these days.
The trillions of bacteria that primarily make up the microbiome are finally gaining the respect they deserve in terms of our health.
We did an extensive look at CBD and probiotics for anxiety or CBD and leaky gut barrier reviews.
Mental health is front and center.
What about schizophrenia?
Researchers were surprised when the scanned the make-up of gut bacteria in healthy controls versus people with schizophrenia:
They were so distinct, in fact, that the researchers were able to tell patients with schizophrenia apart from healthy controls based just on the bacteria in their guts.
Maybe more telling is what happened when they transferred gut bacteria from mice with the mouse equivalent of schizophrenia to healthy mice (called germ-free - no microbiome).
They found that “the mice behaved in a way that is reminiscent of the behavior of people with schizophrenia,”
Nothing happened when gut bacteria were transferred from the same health mice.
We're not surprised as this mirrors other diseases such as Parkinson's.
So...how are the bacteria in our gut affecting something as complex as schizophrenia?
Looking at millions of samples in humans, a study found key differences:
- Patients with schizophrenia had less diversity in gut bacteria
- Patients had different strains of gut bacteria
- Specific strains elevated share a tie with severe depression make-up
- The more significant the alteration of gut bacteria, the more severe the symptoms
https://advances.sciencemag.org/content/5/2/eaau8317
Here's it where it gets downright crazy:
Compared to HCs, germ-free mice receiving SCZ microbiome fecal transplants had lower glutamate and higher glutamine and GABA in the hippocampus and displayed SCZ-relevant behaviors similar to other mouse models of SCZ involving glutamatergic hypofunction.
Let's break that down because it's too important to gloss over.
When they transferred gut bacteria from mice with schizophrenic profiles to germ-free healthy mice (who then went on to show symptoms), there were alterations in the brain.
Alterations in how GABA and glutamate function.
In specific and different areas of the brain which match what we know about schizophrenia!
Just looking at this experiment, you could almost argue (prematurely albeit) that schizophrenia is a disease of our gut.
There were knock-on effects on lipids, the powerful fats that our brain builds and runs on.
Remember how there's a loss of volume in the brains of schizophrenics?
This is where those fats come into play:
Regardless, these findings suggest that the SCZ gut microbiome resulted in lower glycerophospholipid content in the periphery and brains of SCZ microbiota recipient mice, pathologies that are consistent with the synaptic deficits and disconnectivity that are thought to underlie SCZ .
https://advances.sciencemag.org/content/5/2/eaau8317
"Synaptic deficits". "disconnectivity".
Our brain runs on fat! Don't get us started on our steroidal hormones which all derive from cholesterol (see pregnenolone review). We have a whole fats review around the important of omega 3's.
So...we're not getting transfers from infected patients with schizophrenics.
How does this "dysregulation" of the microbiome occur?
A known trigger is a contact with Toxoplasma gondii (from cat feces or litter):
Infection by the neurotropic gut pathogen, Toxoplasma gondii, will elicit an inflammatory GI environment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4294997/
Inflammation causes breaks in our gut barrier (see CBD and gut barrier) which allows pathogens to leak into our bloodstream and even to our nervous system.
All the triggers we saw, to begin with, are inflammatory (infection, stress, trauma, etc).
There are lots of clues pointing to this "autoimmune" angle of schizophrenia:
The earliest interest connecting autoimmunity and schizophrenia stems from a repeated finding of a low prevalence of rheumatoid arthritis in individuals with schizophrenia, beginning with studies in the 1950s and including analyses up to the present.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4294997/
It's not just inflammatory and immune response though...gut bacteria do quite a bit of work for us.
One study looked at the differences:
The study also found that 18 metabolic pathways that were enriched and 14 decreased in schizophrenia relative to controls. Pathways that were significantly altered in schizophrenia were related to environmental information processes such as saccharide, polio, and lipid transport systems.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5503102/
The lipid (fats) pathways are especially fascinating.
A study looked at lipid profiles for people with schizophrenia:
Membrane lipids were not significantly correlated with symptoms at T1, but significantly associated with negative symptoms and functioning at T2 as previously reported.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5000423/
Basically, the "transport" of fats into the cells of our brains was critical.
We saw above how gut bacteria partially govern this process.
And then there are viruses.
One, in particular, stood out from mouth biome studies:
Of the 79 distinct bacteriophage samples that were identified, one, Lactobacillus phage phiadh, was significantly more abundant in schizophrenia cases.
Another study took gut bacteria from human patients with schizophrenia and transplanted them to healthy mice to then began to show signs of the illness.
They even went further to find specific pathways affects.
Some usual suspects came up:
The consistent findings of altered tryptophan-kynurenine metabolism revealed by human serum metabolite analysis, microbiota-based GBM prediction, and mouse studies suggest that this pathway is an important link between schizophrenia and gut microbiota dysbiosis.
https://www.biorxiv.org/content/biorxiv/early/2019/09/19/774265.full.pdf
- Tryptophan (which serotonin is made from and which is downregulated by immune response)
- Kynurenine - we discussed above
We could spend hours and pages here but we'll have to break it out separately.
We need to move on or we'll never get to CBD and other tools.
One more stop...CBD's cousin.
THC and schizophrenia
Enough THC and a person will experience psychosis.
It's a classic psychomimetic (from above).
There's been a long-running battle in research as to the connection between THC and schizophrenia.
- Does THC cause schizophrenia in some people with genetic susceptibility?
- Are people with schizophrenia drawn to THC (self-medication essentially)?
We don't have a clear answer unfortunately but some quick facts.
The next section will also shed some light on the "direction" of cause-effect here.
Early and/or heavy use of cannabis (high THC) may increase risk in people with mental health issues in their family (genetics) or with past trauma (environment).
Of course, few of us know if our mother had the flu in the 2nd trimester.
This risk across the population is estimated to be small. But not zero.
A fascinating study used mice genetically bred to get schizophrenia.
The broke them into different groups and tested the effects of THC.
The results were as expected but a unique piece of information came out of it.
They were able to offset the risk in genetically at-risk mice by boosting key pathways we're absolutely in love with here.
BDNF! (see CBD and BDNF). It's our brain's fertilizer.
Their results:
The introduction of BDNF prevented the development of schizophrenia. Normally, BDNF supports existing neurons and encourages the growth of new synapses and neurons.
https://www.medicalnewstoday.com/articles/317170.php#5
You're going to start to hear a lot about BDNF for mental health going forward. It's literally the linchpin in how SSRI's work (see how SSRI's really work).
This may be the most exciting piece of news as we can actually affect this pathway (besides exercise and meditation).
Borrowing from our last section on gut bacteria:
In a germ-free mice line, decreased expression levels of BDNF and NMDA receptors were found in the cortex and hippocampus.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725071/
Hmmmmm.
We have an entire article on CBD and hippocampus neurogenesis.
This really requires a full exploration but the net effects of THC on symptoms:
Delta-9-tetrahydrocannabinol is associated with transient exacerbation in core psychotic and cognitive deficits in schizophrenia.
https://www.ukcia.org/research/ImplicationsForCognitionPsychosisAddiction.pdf
To be clear...that's THC by itself.
CBD has the exact opposite effect which is standard procedure.
In fact, in studies on psychosis, they'll administer THC to trigger that outcome and CBD to counter it.
See CBD versus THC or why you need CBD if you use Cannabis here.
Our favorite review...Lawyer Up, Sellers of High THC products.
There's lots of research including THC's effect on psychosis there.
We did a huge review on whether people are using THC ro cannabis daily to calm...glutamate! Sound familiar???
Let's finally get to the star of the show.
Everything you've read (bless you) leads to this moment!
Can CBD help with schizophrenia
This may be the most exciting research involving CBD.
Hands down.
We'll dig into all the pathways we discussed above but let's show our cards early.
The study that started it all.
Researchers took 33 patients who were diagnosed at a high risk of psychosis and 19 healthy controls.
Half of the high-risk patients were given a 600 mg dose of CBD isolate. Half were given a placebo.
The results:
The MRI results showed that the irregular brain activity in the three areas we mentioned above (striatum, medial temporal cortex, and midbrain - all tied to psychosis and schizophrenia) normalized to match those of the healthy control subjects.
Furthermore, the clinicians deemed them to no longer appear at risk of psychosis afterward!
The effects of a single dose carried forward for days.
https://jamanetwork.com/journals/jamapsychiatry/article-abstract/2697762
Look...we're 7000 words into this with so many different actors (brain areas, neurotransmitters, gut biome, inflammation, marks of past insults, immune response, etc).
They administer 600 mg of CBD and essentially neutralize the psychosis???
Luckily the study is well designed but we need more research.
Let's look at a follow-up German study comparing CBD and a popular anti-psychotic.
Their results:
At the end of the four-week trial, both groups showed significant clinical improvement in their schizophrenic symptoms, and there was no difference between those getting CBD or amisulpride.
Not only was [CBD] as effective as standard antipsychotics, but it was also essentially free of the typical side effects seen with antipsychotic drugs.
We'll look at CBD versus anti-psychotics below but more on that study.
Here's a list of CBD and schizophrenia clinical trials with lots of additional info:
https://www.psychiatrictimes.com/sites/default/files/PSY0419_005.jpg
What's actually going on?
Let's introduce Anandamide.
Anandamide is our naturally occurring, most prominent endocannabinoid.
It's named after Anand, the Hindu goddess of "Bliss".
Can we just call anti-schizophrenia?
It turns out that the brain responds to the extreme imbalance of schizophrenia by trying to right the ship.
It's main weapon...anandamide.
New studies point to its elevation to schizophrenia but here's the big clue…
- The more the anandamide in the system, the lesser the severity of symptoms.
- Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms.
https://www.ncbi.nlm.nih.gov/pubmed/15354183
So...what does CBD for anandamide in the context of schizophrenia?
Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia.
https://www.nature.com/articles/tp201215
It does this by blocking FAAH which eats up anandamide in the body.
Check out FAAH and the woman who can't feel pain, anxiety, or depression.
We're assuming schizophrenia also shows no risk for her.
Let's start to look at some of the pathways we discussed above.
We'll hit highlights on these:
- CBD and serotonin for schizophrenia
- CBD and dopamine for schizophrenia
- CBD and GABA/Glutamate for schizophrenia
- CBD and neuroinflammation
- CBD and microglia
- CBD and gut biome
- CBD and kynurenine
Lots to cover.
CBD and serotonin for schizophrenia
CBD has powerful effects to balance serotonin function is essential.
The net effect:
Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6319597/
The keyword there is "modulate". Not boost or reduce. So after injury (a form of stress), CBD calmed anxiety and pain sensitivity by supporting serotonin when low.
Check out CBD versus SSRI's for serotonin to understand why this is so important.
What about dopamine, a key player with schizophrenia?
CBD and dopamine for schizophrenia
Interestingly, most of the research on dopamine stems for research on….you guessed it...schizophrenia.
The results again revolve around balance:
However, evidence has demonstrated that CBD strongly modulates the mesolimbic dopamine (DA) system and may possess promising antipsychotic properties.
https://www.ncbi.nlm.nih.gov/pubmed/28185872
There's that word again…"modulate". I.e. balance.
They show the interaction with serotonin and dopamine as well.
Their net assessment:
Together with clinical evidence showing that CBD may normalize affective and cognitive deficits associated with schizophrenia, CBD may represent a promising treatment for schizophrenia, acting through novel molecular and neuronal mesolimbic substrates.
Next up...the gas and brake pedal in the brain.
CBD and GABA/Glutamate for schizophrenia
Glutamate (remember the NMDA receptors??) figure strongly into schizophrenia pathways.
Remember that CBD was basically discovered as a remarkable treatment for seizures, the poster child for GABA and Glutamate imbalance (too much gas pedal, not enough brake).
We'll start easy and show just how technical newer studies are getting.
Preclinical evidence suggests that one aspect of the polypharmacy of CBD is that it modulates brain excitatory glutamate and inhibitory γ-aminobutyric acid (GABA) levels.
https://www.ncbi.nlm.nih.gov/pubmed/30758329
Our favorite word…" modulates".
Now...just to show where the level of research is recently.
Basically, researchers are finding that too much activity in our endocannabinoid system may be a driving force for schizophrenia.
This is why THC in excess can trigger psychosis.
CBD acts as a negative modulator on this system. It's a rubber band that pulls it back when it pushes too far.
The effect in terms of GABA/glutamate from this action prompted by infection?
CBD treatment attenuated poly I:C-induced deficits in cannabinoid CB1 receptor binding in the PFC and glutamate decarboxylase 67, the enzyme that converts glutamate to GABA, in the HPC.
https://www.ncbi.nlm.nih.gov/pubmed/31202911
Goodness...that's a mouthful.
Essentially, CBD reigns in an activity that causes an imbalance between glutamate and GABA in a very important part of the brain for schizophrenia...the prefrontal cortex (PFC).
This was caused by ...immune system response to EARLY infection!
Check out CBD and GABA for the info there.
Next up...inflammatory pathways.
CBD and neuroinflammation
Just a few of many examples (more can be found at our CBD and neuroinflammation review".
Interestingly, the higher inflammation, the worst the severity of schizophrenia symptoms such as cognitive tasks.
CBD's result:
Overall, inflammatory-based models of cognitive impairment consistently show that short-term and long-term 542 CBD administration can attenuate deficits in spatial learning and memory, recognition memory and associative 543 learning [60-62], which are cognitive domains affected in schizophrenia, as identified by MATRICS.
http://ro.uow.edu.au/cgi/viewcontent.cgi?article=2037&context=ihmri
That's the cognitive or thinking side of the equation.
And then there are the social effects of schizophrenia. Withdrawal and retrenchment.
CBD there:
In conclusion, chronic CBD administration can attenuate the social interaction and cognitive deficits induced by prenatal poly I:C infection. These novel findings present interesting implications for the potential use of CBD in treating the cognitive deficits and social withdrawal of schizophrenia.
https://www.ncbi.nlm.nih.gov/pubmed/28230072
There's that prenatal infection piece again! Folks...they can give animals their version of schizophrenia later in life just by introducing bacteral signatures early on.
Studies looked at CBD after strokes since this is a period of intense brain inflammation...maybe the most aside from sepsis.
CBD helped to calm the inflammatory storm and actually spur repair (BDNF!!!):
In addition, ischemic mice treated with CBD exhibited an increase in the hippocampal brain-derived neurotrophic factor (BDNF) protein levels. CBD also stimulated neurogenesis and promoted dendritic restructuring in the hippocampus of BCCAO animals.
https://www.sciencedirect.com/science/article/pii/S0278584616302524
Part of this was calming microglia activation. Let's go there now.
CBD and microglia
Remember the "priming" of microglia and our immune response from early exposure?
Read this…
Moreover, CBD administration at the time of viral infection exerts long-lasting effects, ameliorating motor deficits in the chronic phase of the disease in conjunction with reduced microglial activation and pro-inflammatory cytokine production.
https://www.sciencedirect.com/science/article/pii/S0969996113001939
Another study put it simply:
Cannabinoids regulate the brain–immune axis and inhibit microglial cell activation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729885/
Look...immune response and microglia are the new superstars for mental health diseases.
Look at what happens when they inject the amyloid plaques into the brains and then follow up with CBD:
Finally, both CBD and WIN, after subchronic administration for 3 weeks, were able to prevent learning of a spatial navigation task and cytokine gene expression in β-amyloid-injected mice.
https://www.ncbi.nlm.nih.gov/pubmed/21350020
Down south.
CBD and gut biome
All inflammatory processes have some roots in the gut and CBD operates there as well.
We did full reviews at CBD and probiotics for anxiety and CBD and the leaky gut barrier.
Just a few looks at CBD's effect on inflammation in the gut (key to bacteria/virus leaking out into the body...and brain!!)
Pick a gut inflammatory disease.
Ulcerative Colitis? Sure.
CBD targets enteric reactive gliosis, counteracts the inflammatory environment induced by LPS in mice and in human colonic cultures derived from UC patients.
https://www.ncbi.nlm.nih.gov/pubmed/22163000
In general, to wrap up gut inflammation, glia cells, bacteria response, and CBD:
A study in a lipopolysaccharide-induced model suggested that CBD, which is known to act as GPR55 antagonist [46], inhibits GI inflammation by controlling the inflammatory response and the activation of enteric glial cells.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5388177/
- Lipopolysaccharide (LPS) is the signature protein for bacteria
- GI - our gut
- Glia cells - gut immune responders (like the microglia in the brain)
Finally...that kynurenine angle.
CBD and kynurenine
This really requires a full, breakout review.
Basically, kynurenine and serotonin share the same raw material...tryptophan.
In times of immune response (infection, stress, trauma), the body shifts from serotonin production to kynurenine and/or reduction in the raw material tryptophan itself.
This is to starve out bacteria and viruses of their raw building material (tryptophan as well).
So...the net of this is…
The more kynurenine you have, the less serotonin.
This whole shift is triggered by inflammation (be it from infection, priming, or stress):
Proinflammatory cytokines induce IDO under stress, promote the KYN pathway, deprive the 5-HT pathway of TRP, and reduce 5-HT synthesis.
https://www.tandfonline.com/doi/abs/10.1080/10253890701754068
Remember how people with schizophrenia have higher levels of kynurenine?
What does CBD do there (besides bringing down inflammation)?
Researchers looked at CBD's effect on immune cells triggered by pathogen:
The highest concentration tested (16 μM) almost completely inhibited IDO mRNA expression induced by PHA. CBD was also shown to inhibit LPS stimulation of THP-1 cell IDO activity (IC50 = 0.9 μM).
https://link.springer.com/article/10.1007/s13311-015-0377-3
Translation, please.
The higher the level of CBD, the greater the reduction in this shift to kynurenine.
A downshift if you will of our immune response (which is heightened in schizophrenia).
It hits the driver which is IDO.
We'll leave with this clinical trial of CBD and schizophrenia:
After 6 weeks of treatment, compared with the placebo group, the CBD group had lower levels of positive psychotic symptoms (PANSS: treatment difference=−1.4, 95% CI=−2.5, −0.2) and were more likely to have been rated as improved (CGI-I: treatment difference=−0.5, 95% CI=−0.8, −0.1) and as not severely unwell (CGI-S: treatment difference=−0.3, 95% CI=−0.5, 0.0) by the treating clinician.
https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2017.17030325
Check out the chart which showed roughly 30% as very much or much improved by the treating clinician here:
https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2017.17030325#F2
Another 50% showed improvement.
We've covered a great deal. Of course, this is just a smattering of research out there but it points to many of the pathways of schizophrenia affected by CBD.
Let's look at some other tools we've found during the course of our study.
Other promising tools for schizophrenia
If I could turn back the clock, I would have given all of these to my brother.
Most of these revolve around calming immune, inflammatory, and oxidative pathways.
Here are additional resources to research:
- NAC - big booster of glutathione, our primary anti-oxidant (see CBD and glutathione) Purchase here
- Glycine - competes with kynurenine and is very fascinating
- Berberine - powerful gut biome remodeler. Full review here. Purchase here
- B complex (methylated if MTRR or MTHR which is 40% of the population) Purchase here
- Pregnenolone - the brain's natural pushback to excessive THC
- Vitamind D and seteroidal hormones - immune managers extraordinaire!
- Medicinal mushroooms - powerful immune regulators
Remember, kynurenine is a by-product of an overactive immune response!
Let's look at the traditional meds.
CBD versus antipsychotics for schizophrenia
We saw the German study where CBD was as effective as amisulpride.
Amisulpride (US version)
How does it work?
Amisulpride is believed to work by reducing signaling via the dopamine D2 receptor.
https://en.wikipedia.org/wiki/Amisulpride
This drug ranked high for its effect on schizophrenia symptoms:
In a 2013 study in a comparison of 15 antipsychotic drugs' ineffectiveness in treating schizophrenic symptoms, amisulpride was ranked second and demonstrated high effectiveness. 11% more effective than olanzapine (3rd), 32-35% more effective than haloperidol, quetiapine, and aripiprazole, and 25% less effective than clozapine (1st).
Here's the issue. The side effects can be brutal.
Here's the list:
https://www.medicines.org.uk/emc/product/3963/pil
Dopamine is a workhorse neurotransmitter with effects across a range of bodily functions.
The effects on sleep and weight gain are the most troublesome.
And...CBD was found to be as effective as it in the German study!
What about the #1 rated drug for schizophrenia..clozapine (generally sold as Clozaril).
Its effect are more varied across dopamine, serotonin, and GABA pathways.
Remember...our brain chemistry is an orchestra and they all interact in complex ways with dozens if not 100's of other chemicals.
For that reason, the side effect list for Clozaril is equally involved and varied:
https://www.rxlist.com/clozaril-side-effects-drug-center.htm#overview
My brother tried a few different medications but it made him gain weight and sleep all the time.
As for clozapine versus CBD, one study injected mice with a substance (MK801) that blocks NMDA receptors.
This results in schizophrenia-like symptoms in the mice.
Our findings show that a 2-week treatment with the NMDA receptor antagonist MK801 impairs social interaction and novel object recognition, which have been associated with negative and cognitive symptoms of schizophrenia, respectively.
They then looked at social interaction and object recognition.
The results?
Repeated CBD or clozapine treatment reversed these impairments. CB1 and CB2 antagonists (AM251 and AM630, respectively) failed to change the CBD effect. However, its effect was blocked by pretreatment with the 5HT1A receptor antagonist WAY100635.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5887392/
It's interesting because they found that it wasn't due to cannabinoid receptors but actually due to serotonin function!
Remember that serotonin is on a see-saw with kynurenine (kicked up by the immune system).
Learn about CBD and serotonin versus SSRI's here.
Let's go back to the German study.
These were patients with a schizophrenia prior diagnosis who had been a course of treatment with clozapine.
In a double-blind test with a placebo, they then tested CBD against amisulpride.
The specific results:
Comparison (modified intention-to-treat) of the clinical effects of amisulpride and cannabidiol revealed no relevant difference between the two treatments.
Check out the study...it's very well-structured.
Their net conclusion:
These results suggest that cannabidiol is as effective at improving psychotic symptoms as the standard antipsychotic amisulpride.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3316151/
But what about side effects? Both amisulpride and clozapine have pretty significant baggage there.
Compared with amisulpride, we found that treatment with cannabidiol was associated with significantly fewer extrapyramidal symptoms (P=0.006; Figure 3a), less weight gain (P=0.010; Figure 3b), and lower prolactin increase—a predictor of galactorrhoea and sexual dysfunction (P<0.001; Figure 3c).
Check out the comparison chart on the page.
The side effects and weight gain actually go DOWN by day 28 after a brief increase at day 14.
The amisulpride side effect and weight gain increase significantly to day 14 and continues to increase (especially on the weight gain side).
Check out our review on whether CBD is safe here.
The common side effects of CBD:
- Lower blood pressure
- Dry mouth
- Lightheadedness
- Drowsiness
Most of these tend to recede with longer periods of use.
Interestingly, CBD during the day can be a wake-promoting agent (see Can I take CBD in the Middle of the Day?)
The review of clinical trials in terms of safety:
The review by Bergamaschi et al. mentions three acute human studies that have demonstrated the CBD antipsychotic effect without any adverse effects being observed.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569602/
Another clinical trial had this to say about the side effect and safety of CBD:
Only one-third of the patients in each group reported treatment-emergent adverse events. The majority of these were mild and resolved spontaneously, with no significant differences in frequency between the CBD and placebo groups.
https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2017.17030325
"No significant differences in frequency between CBD and placebo"
Seeing this above, it's really hard to understand the current course of treatment...in my humble opinion.
Some practical questions.
Can I take CBD with my medications for schizophrenia
First, always work with your doctor or naturopath with ANY supplements!
CBD uses the same pathway in the liver at 60% of medications.
It may increase or decrease the availability of those medications in your system.
The general rule of thumb is 4 hours away from any medications but antipsychotics are very powerful.
We looked at how CBD helps to normalize dopamine, serotonin, and GABA/glutamate systems.
Since the anti-psychotics are reducing/boosting levels in these pathways, CBD might offset this or help to constrain the activity.
We don't have good research on that yet.
Work with your doctor.
We have lots of clients slowly integrate CBD to wean off benzos or SSRI's.
A slow rotation of the two.
Find a good naturopath or doctor (who is keeping up with research) that will help you with this process.
CBD for paranoia
This is the hardest and seemingly most intractable part of schizophrenia.
Unfortunately, it afflicts the vast majority of people with the disease.
We stumbled on a study with CBD and paranoia a few months ago and we've been waiting all this time to bring it up.
Let's take our first clue from THC-triggered paranoia.
Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment.
https://www.ncbi.nlm.nih.gov/pubmed/23042808
Paranoia falls under the heading of "positive" symptoms of schizophrenia.
These generally include paranoia, hallucinations, voices, and the like.
These contrast with the negatives (lack of energy, social withdrawal, low mood, etc)
The effects of CBD on these "positive" symptoms from a double-blind, clinical trial?
Positive psychotic symptoms (measured using the PANSS positive subscale) were significantly reduced from baseline to end of treatment in the CBD group compared with the placebo group.
https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2017.17030325
Check out the chart here:
https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2017.17030325#T2
This is very exciting as the first step to getting help is to break through this paranoia.
To ever more practical questions.
How much CBD to take for schizophrenia
Let's look at research for this question.
First, a general starting dose to test effects is 25-30 mg.
You wouldn't expect any benefit mirroring what research is showing above but it's just to see how a specific body responds.
As for the research, they're using between 600 - 800 mg doses daily.
One big study started everything had a one time 600 mg dose which had lasting effects.
The follow-up, more robust clinical trials generally use 600-800mg doses per day over a longer period of time.
Here's the issue...this is expensive.
We've specifically priced our CBD at the lowest on the market (3 cents per mg for the 6000 mg bottle) because of this. Before discounts up to 50%
There are people suffering and even at the 6000 mg bottle, that's only going to last 10 days.
We can try to work with people on a subscription discount who find benefits from CBD.
We don't want people to suffer so please check with us.
We've been there (founder's story is here) and I know first hand how brutal schizophrenia can be.
Check with us at support@indigonaturals.net or via chat window below.
Our goal is to eventually roll out a trial at our cost with the CBD for people on the street (along with the other tools we mentioned above).
That's my dream anyway. Some important items in terms of kind of CBD.
What's the best kind of CBD for schizophrenia
Of course, the basics apply for ANY CBD use:
- Organically grown in the US at an FDA certified farm
- 3rd party tested (we test both biomass and finished product separately)
- THC free (THC can actually cause psychosis)
- No pesticides
- No mold
- No heavy metals
- No bacteria
That's just the starting point for us.
Here's the big deal we need to look at.
The vast majority of brands out there are pushing full-spectrum CBD.
There's no research for this and if you haven't noticed, we make our decisions based on research.
The other issue is more pressing.
Roughly 40-60% of people have histamine issues.
There's a known correlation between asthma and schizophrenia:
After adjusting for potential confounding factors, asthma was associated with a significantly greater hazard ratio for incident schizophrenia 1.40.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5369699/
That's a 40% increase in risk!
Asthma is a known result of histamine overactivity.
Here's the deal...histamine is a powerful inflammatory agent in the brain.
The very opposite direction we want to go to!
There are more clues coming with new research:
In clinical studies, the levels of N-tele-methylhistamine, a major brain histamine metabolite, were elevated in the cerebrospinal fluid of schizophrenics.
https://www.ncbi.nlm.nih.gov/pubmed/15334189
By the way, the main anti-psychotic medications increase histamine turnover...a way to get rid of it.
The last thing we want is all that plant material in full-spectrum CBD.
We want CBD isolate.
Why?
Almost all research on CBD and schizophrenia is CBD isolate.
The research is pretty promising so unless we see something different, CBD Isolate is the way to go.
Check out CBD isolate versus full spectrum for anxiety to understand the difference.
Finally...if you've come this far, Thank you.
Our exhaustive effort to shine a light on CBD's effect on schizophrenia and psychosis is a reaction to my ability to reach my brother.
I'm literally planning to sneak CBD oil into cookies at this point.
That makes it all worthwhile.
Be well. Be informed. Take care of each other.
Related Research:
CBD and paranoia
CBD and early trauma
CBD and immune system for mental health
Always work with a doctor or naturopath with any supplement!
The information provided here is not intended to treat an illness or substitute for professional medical advice, diagnosis, or treatment from a qualified healthcare provider.